What is a Hip Labral Tear?
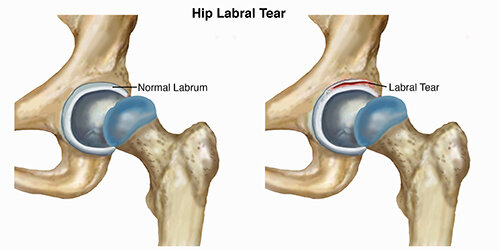
A hip labral tear occurs when there is damage to the labrum (ring of cartilage) within the hip joint. The hip joint is where the thigh bone (femur) meets the pelvis (ilium). It is described as a ball-and-socket joint. This design allows the hip to move in several directions. The bony hip socket is surrounded by the labrum, which provides additional stability and shock absorption to the hip joint.
A labral tear results when a part of the labrum separates or is pulled away from the socket. Most commonly, a labral tear is the result of repetitive stress (loading) causing irritation to the hip, often due to long-distance running or performing repeated, sharp, sports movements, such as twisting and cutting.
Repetitive loading is more likely to result in injury to the labrum when there are bony abnormalities at the hip joint. For example, hip impingement is a condition resulting in hip pain due to abnormal bony contact between the ball and socket. As the hip is moved into specific positions, this bony contact can place greater stress on the labrum.
Hip labral tears may result from a combination of several different variables, including:
Bony abnormalities in the hip joint (hip impingement)
Hip muscle tightness
Hip muscle weakness
An unstable hip joint
Improper technique when performing repetitive activities
Participation in sports that require distance running, or repetitive twisting and cutting
Typical wear-and-tear over time
Once torn, the labral tissue in the hip does not have the ability to heal on its own. There are surgical procedures to remove or repair torn labral tissue; however, treatment for a labral tear often begins with a course of physical therapy.
Nonsurgical treatment efforts are focused on addressing symptoms by maximizing the strength and mobility of the hip to minimize the stress placed on the injured area. In some cases, patients are able to achieve a satisfactory level of activity without surgery.
Surgical interventions are available to clean out the hip joint, and repair or reconstruct the torn labral tissue. Following surgery, patients will complete several months of physical therapy to regain function of the hip.
How Does it Feel?
Many people have labral tears in the hip and do not experience symptoms; however, some labral tears can result in significant pain or limitations. Pain in the front of the hip or in the groin resulting from a hip labral tear can cause an individual to have limited ability to stand, walk, climb stairs, squat, or participate in recreational activities.
With a labral tear, you may experience:
A deep ache in the front of your hip or groin, often described by the "C sign." (People make a "C" with the thumb and hand, and place it on the fold at the front and side of the hip to locate their pain.)
Painful clicking or "catching" with hip movements; the feeling of something painful stuck in the hip or blocking hip motion.
Pain that increases with prolonged sitting or walking.
A sharp pain in the hip or groin when squatting.
Pain that comes on gradually rather than with one specific episode.
Weakness in the muscles surrounding the hip, or a feeling of the hip “giving way.”
Stiffness in the hip.
How Is It Diagnosed?
Your physical therapist will begin your evaluation by gathering information about your condition and medical history. Although a hip labral tear may be the result of a single injury, it most likely is a condition that develops as a consequence of repetitive irritation in the hip. Your physical therapist may ask you to describe:
Your current symptoms and how they affect your activities in a typical day
Any pain you are experiencing, its intensity and location, and how it may vary during the day
What activities you may be unable to do or have difficulty completing
What activities aggravate your symptoms, and how you reduce the level of your discomfort
Prior injury occurrences before your symptoms began
Other health care professional visits and any tests received
Your physical examination will focus on the region where your symptoms are occurring, but also include other areas that may have been affected as your body adjusted to pain. Your physical therapist may watch you walk, step onto a stair, squat, or balance on one leg.
Your physical therapist will gently but skillfully palpate (touch) the front, side, and back of your hip to determine exactly where it is most painful. The therapist will assess the mobility and strength of your hip and other regions of the body to determine the areas that require treatment.
Following the interview and physical examination, your physical therapist will discuss the findings with you and, through mutual collaboration, develop an individualized treatment program to begin your recovery.
Your physical therapist also may refer you to an orthopedic physician who specializes in hip injuries for diagnostic imaging (ie, X-ray, MRI). An X-ray helps to identify any bony abnormalities, such as those that occur with hip impingement, which may be contributing to your pain. An MRI helps to identify a labral tear.
How Can a Physical Therapist Help?
When you have been diagnosed with a hip labral tear, your physical therapist will work with you to develop a plan to help achieve your specific goals. To do so, your therapist will select treatment strategies in any or all of the following areas:
Education. Your physical therapist will work with you to identify and change any external factors causing your pain, such as exercise selection, footwear, or the amount of exercises you perform.
Pain management. Many pain-relief strategies may be implemented; the most beneficial strategy to alleviate hip pain is to apply ice to the area and to decrease or eliminate specific activities causing your symptoms. Your physical therapist will identify specific movements that aggravate the inside of your hip joint, and design an individualized treatment plan for you, beginning with a period of rest, and gradually adding a return to certain activities as appropriate. Physical therapists are experts in prescribing pain-management techniques that reduce or eliminate the need for medication, including opioids.
Manual therapy. Your physical therapist may apply hands-on treatments to gently move your muscles and joints to decrease your pain and improve motion and strength. These techniques often address areas that are difficult to treat on your own.
Movement reeducation. Your back and hip may be moving improperly, causing increased tension at the hip joint. Your physical therapist may teach you self-stretching techniques for the lower body to decrease tension and help restore normal motion in the back, hip, and leg. There are, however, certain hip motions to avoid following an injury to the hip labrum. Your physical therapist will carefully prescribe exercises that improve your range of motion while protecting the area that has the labral tear.
Muscle strengthening. Muscle weaknesses or imbalances can be the cause or the result of hip pain. Based on your specific condition, your physical therapist will design a safe, individualized, progressive resistance program for you, likely including your core (midsection) and lower extremity. You may begin by performing strengthening exercises while lying down, and advance to performing exercises in a standing position. Your physical therapist will choose what exercises are right for you.
Functional training. Once your pain, strength, and motion improve you will be able to safely transition back into more demanding activities. To minimize tension on the hip, it is important to teach your body safe, controlled movements. Based on your own unique movement assessment and goals, your physical therapist will create a series of activities to help you learn how to use and move your body correctly and safely. Your therapist also will discuss specific positions and activities that should be avoided or modified to protect your hip.
Can this Injury or Condition be Prevented?
Repetitive motion, such as sports or long-distance running, can create the risk of sustaining a labral injury. It is imperative to be aware of any hip pain that you experience, particularly with sitting and squatting, as these are signs of a potential hip injury. Identifying and addressing these injuries early is helpful in their treatment. A physical therapist can help an active individual learn proper body movements to lessen the possibility of injury.
After recovering from a hip labral tear, it is important to continue the lower-extremity mobility and muscle strengthening practices taught to you by your physical therapist, to help reduce the risk of further irritation or injury. In some cases, complete avoidance of the activity that contributed to the symptoms may be recommended.
Real Life Experiences
Erin is a 27-year-old accountant who is training for an upcoming half-marathon. She runs 5 days a week and also enjoys performing weight training and strengthening exercises 2 to 3 days a week. Over the past 2 weeks, Erin has begun to experience an achy pain in the front of her right hip. Her pain is worse after running, and while sitting in her car and at her desk. She also experiences occasional "catching" in her hip when reaching forward to pick up her 1-year-old daughter.
Erin is concerned about the pain she feels between runs and her inability to sit without discomfort. She is worried about her ability to perform daily activities, care for her daughter, and train for her upcoming race. She consults her physical therapist.
Erin’s physical therapist conducts a comprehensive assessment of her current symptoms and her health history. She assesses Erin’s motion, strength, balance, movement, and running mechanics. She skillfully palpates (touches) the front, side, and back of Erin’s hip to determine the precise location of her pain. Erin describes her typical daily running routine, her stretching routine, and her footwear. Based on these findings, her physical therapist suspects an injury to her labrum within her hip joint.
Because Erin’s hip is so tender, her physical therapist refers her to an orthopedic surgeon. The surgeon confirms the diagnosis of a hip labral tear. Erin and her surgeon discuss treatment options; the decision is made for nonoperative management of the condition, with a 2-month period of physical therapy.
Erin and her physical therapist work together to establish short- and long-term goals and identify immediate treatment priorities, including icing and activity modification to decrease her pain as well as gentle hip-strengthening exercises. Her physical therapist also teaches her a home-exercise program to perform daily to help speed her recovery.
Together, they outline a 4-week rehabilitation program. Erin sees her physical therapist 1 to 2 times each week; she assesses Erin’s progress, performs manual therapy techniques, and advances her exercise program as appropriate. She advises Erin on exercise and activity modifications that will enhance her recovery. Erin maintains her daily exercise routine at home.
After 6 weeks, Erin's hip no longer "catches" when she bends forward, and she only experiences periodic mild discomfort when sitting or running.
On the day of the half-marathon, Erin runs pain free—and is proud to high five her husband and her little daughter at the finish line!
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat a labral injury in the hip. However, you may want to consider:
A physical therapist who is experienced in treating people with hip labral injuries or tears, and hip impingement. Some physical therapists have a practice with an orthopedic or musculoskeletal focus.
A physical therapist who is a board-certified clinical specialist, or who completed a residency or fellowship in orthopedic or sports physical therapy. This physical therapist has advanced knowledge, experience, and skills that may apply to your condition.
You can find physical therapists who have these and other credentials by using Find a PT, the online tool built by the American Physical Therapy Association to help you search for physical therapists with specific clinical expertise in your geographic area.
General tips when you're looking for a physical therapist (or any other health care provider):
Get recommendations from family and friends or from other health care providers.
When you contact a physical therapy clinic for an appointment, ask about the physical therapists' experience in helping people who have hip labral injury or hip impingement.
During your first visit with the physical therapist, be prepared to describe your symptoms in as much detail as possible, and describe what makes your symptoms worse.
Further Reading
The American Physical Therapy Association (APTA) believes that consumers should have access to information that could help them make health care decisions and also prepare them for a visit with their health care provider.
The following articles provide some of the best scientific evidence related to physical therapy treatment of labral tears in the hip. The articles report recent research and give an overview of the standards of practice both in the United States and internationally. The article titles are linked either to a PubMed* abstract of the article or to free full text, so that you can read it or print out a copy to bring with you to your health care provider.
McGovern RP, Martin RR, Kivlan BR, Christoforetti JJ. Non-operative management of individuals with non-arthritic hip pain: a literature review. Int J Sport Phys Ther. 2019;14(1): 135–147. Free Article.
Pennock AT, Bomar AD, Johnson KP, Randich K, Upasani W. Nonoperative management of femoroacetabular impingement: a prospective study. Am J Sports Med. 2018;46(14):3415–3422. Article Summary in PubMed.
Griffin DR, Dickenson EJ, O’Donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50:1169–1176. Free Article.
*PubMed is a free online resource developed by the National Center for Biotechnology Information (NCBI). PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine’s MEDLINE database
Authored by Allison Mumbleau, PT, DPT, SCS. Revised by Jennifer Bagwell, PT, PhD, DPT, member of APTA's Academy of Orthopaedic Physical Therapy. Reviewed by an APTA section liaison.