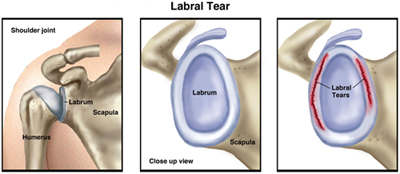
An unstable shoulder joint can be the cause or the result of a labral tear. "Labral" refers to the ring of cartilage (glenoid labrum) that surrounds the base of the shoulder joint. Injuries to the labrum are common, can cause a great deal of pain, and may make it hard to move your arm. A labral tear can occur from a fall or from repetitive work activities or sports that require you to use your arms raised above your head. Some labral tears can be managed with physical therapy; in severe cases, surgery may be required to repair the torn labrum.
The ring of cartilage called the glenoid labrum provides extra support for the shoulder joint, helping to keep it in place. A shoulder labral tear occurs when part of this ring is disrupted, frayed, or torn. Tears may lead to shoulder pain, an unstable shoulder joint, and, in severe cases, dislocation of the shoulder. Likewise, a shoulder dislocation can result in labral tears.
When you think of the shoulder joint, picture a golf ball (the head of the upper-arm bone, or humerus) resting on a golf tee (the glenoid fossa, a shallow cavity or socket located on the shoulder blade, or scapula). The labrum provides a rim for the socket (golf tee) so that the humerus (golf ball) does not easily fall off. If the labrum is torn, it is harder for the humerus to stay in the socket. The end result is that the shoulder joint becomes unstable and prone to injury.
Because the biceps tendon attaches to the shoulder blade through the labrum, labral tears can occur when you put extra strain on the biceps muscle, such as when you throw a ball. Tears also can result from pinching or compressing the shoulder joint, when the arm is raised overhead.
There are 2 types of labral tears:
Traumatic labral tears usually occur because of a single incident, such as a shoulder dislocation or an injury from heavy lifting. People who use their arms raised over their heads—such as weight lifters, gymnasts, and construction workers—are more likely to experience traumatic labral tears. Activities where the force occurs at a distance from the shoulder, such as striking a hammer or swinging a racquet, can cause a traumatic labral tear. Falling on an outstretched arm also can cause this type of tear.
Nontraumatic labral tears most often occur because of muscle weakness or shoulder joint instability. When the muscles that stabilize the shoulder joint are weak, more stress is put on the labrum, leading to a tear. People with nontraumatic tears tend to have more "looseness" or greater mobility throughout all their joints, which might be a factor in the development of a tear.
How Does it Feel?
A shoulder labral tear may cause you to feel:
Pain over the top of your shoulder
"Popping," "clunking," or "catching" with shoulder movement, because the torn labrum has "loose ends" that are flipped or rolled within the shoulder joint during arm movement, and may even become trapped between the upper arm and shoulder blade
Shoulder weakness, often on one side
A sensation that your shoulder joint will pop out of place
How Is It Diagnosed?
Not all shoulder labral tears cause symptoms. In fact, when tears are small, many people function without any symptoms. However, healing may be difficult due to the lack of blood supply available to a torn labrum. The shoulder with a labral tear may pop or click without being painful, but if the tear progresses, it is likely to lead to pain and weakness.
If your physical therapist suspects that you have a labral tear, your physical therapist will review your health history and perform an examination that is designed to test the condition of the glenoid labrum. The tests will place your shoulder in positions that may recreate some of your symptoms, such as "popping," "clicking," or mild pain, to help your physical therapist determine whether your shoulder joint is unstable. Magnetic resonance imaging (MRI) also may be used to complete the diagnosis. Some labral tears may be difficult to diagnose with certainty without arthroscopic surgery. Your physical therapist may consult with an orthopedic surgeon if necessary.
How Can a Physical Therapist Help?
When shoulder labral tears cause minor symptoms but don’t cause shoulder instability, they usually are treated with physical therapy. Your physical therapist will educate you about positions and activities to avoid, and tailor a treatment plan for your recovery. Your treatment may include:
Manual therapy. Your physical therapist may provide gentle manual (hands-on) therapy to decrease your pain and begin to restore movement in the shoulder area.
Strengthening exercises. Improving the strength of the muscles of the shoulder will help you decrease the stresses placed on the torn labrum and allow for better healing. Your physical therapist may design rotation exercises that target the muscles of the shoulder joint, and shoulder-blade (scapular) exercises to provide stability to the shoulder joint itself.
Stretching exercises. An imbalance in the muscles or a decrease in flexibility can result in poor posture or excessive stress within the shoulder joint. Your physical therapist may prescribe stretching exercises—such as gentle stretches of the chest (pectoralis) muscles—to improve the function of the muscles surrounding the shoulder. Your physical therapist also may introduce middle-back (thoracic) stretches to allow your body to rotate or twist to the side, so the shoulder joint doesn’t have to stretch further to perform tasks, such as swinging a racquet or golf club.
Postural exercises. Your physical therapist will assess your posture, and teach you specific exercises to ensure your shoulders are positioned properly for daily tasks. A forward-head and rounded-shoulder posture puts the shoulders at risk for injury.
Education. Education is an important part of any physical therapy treatment plan. Your physical therapist will help you understand your injury, the reasons for modifying your activities, and the importance of doing your exercises to decrease your risk of future injury.
Home-exercise program. A home-exercise program is an important companion to treatment in the physical therapy clinic. Your physical therapist will identify the stretching and strengthening exercises that will help you steadily improve your shoulder function and meet your work, home, and activity goals.
Following Surgery
In more severe cases, when conservative treatments are unable to completely relieve the symptoms of a labral tear, surgery may be required to reattach the torn labrum. Following surgery, your physical therapist will design a treatment program based on your specific needs and goals, and work with you to help you safely return to your daily activities.
A surgically repaired labrum takes 9 to 12 months to completely heal. Immediately following surgery, your physical therapist will teach you ways to avoid putting excessive stress or strain on the repaired labrum.
As the labrum heals, your physical therapist will introduce resistance and strengthening exercises, such as those listed above, to your treatment plan, to address your specific needs, and help you slowly and safely return to performing daily tasks that require force or lifting. Your physical therapist is trained to gradually introduce movements in a safe manner to allow you to return to your usual activities without re-injuring the repaired tissues.
Can this Injury or Condition be Prevented?
Forceful activities performed with the arms raised overhead may increase the likelihood of developing a labral tear. To avoid putting excessive stress on the labrum, you need to develop strength in the muscles that surround the shoulder and scapula. Your physical therapist can:
Design exercises to help you strengthen your shoulder and shoulder blade muscles
Show you how to avoid potentially harmful positions
Train you to properly control your shoulder movement and modify your activities to reduce your risk of sustaining a labral injury
Provide posture education to help you avoid placing unnecessary forces on the shoulder
Help you increase your shoulder and middle-back flexibility
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat patients who have a shoulder labral tear, but you may want to consider:
A physical therapist who is experienced in treating people with musculoskeletal problems. Some physical therapists have a practice with an orthopedic focus.
A physical therapist who is a board-certified clinical specialist or who completed a residency or fellowship in orthopedics physical therapy has advanced knowledge, experience, and skills that may apply to your condition.
You can find physical therapists who have these and other credentials by using Find a PT, the online tool built by the American Physical Therapy Association to help you search for physical therapists with specific clinical expertise in your geographic area.
General tips when you're looking for a physical therapist (or any other health care provider):
Get recommendations from family and friends or from other health care providers.
When you contact a physical therapy clinic for an appointment, ask about the physical therapists' experience in helping people with labral tears.
During your first visit with the physical therapist, be prepared to describe your symptoms in as much detail as possible, and say what makes your symptoms worse.
Further Reading
The American Physical Therapy Association (APTA) believes that consumers should have access to information that could help them make health care decisions and also prepare them for their visit with their health care provider.
APTA has determined that the following articles provide some of the best scientific evidence for how to treat labral tears. The articles report recent research and give an overview of the standards of practice for treatment both in the United States and internationally. The article titles are linked either to a PubMed* abstract of the article or to free access of the full article, so that you can read it or print out a copy to bring with you to your health care provider.
Mazzocca AD, Cote MP, Solovyova O, et al. Traumatic shoulder instability involving anterior, inferior, and posterior labral injury: a prospective clinical evaluation of arthroscopic repair of 270° labral tears. Am J Sports Med. 2011;39:1687-1696. Article Summary on PubMed.
Dodson CC, Altchek DW. SLAP lesions: an update on recognition and treatment. J Orthop Sports Phys Ther. 2009;39:71-80. Article Summary on PubMed.
Keener JD, Brophy RH. Superior labral tears of the shoulder: pathogenesis, evaluation, and treatment. J Am Acad Orthop Surg. 2009;17:627-637. Article Summary on PubMed.
*PubMed is a free online resource developed by the National Center for Biotechnology Information (NCBI). PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine’s MEDLINE database.”
Authored by Charles Thigpen, PhD, PT, ATC and Lane Bailey, PT, DPT, CSCS. Reviewed by the MoveForwardPT.com editorial board.