Impact of sedentarism due to the COVID-19 home confinement on neuromuscular, cardiovascular and metabolic health: Physiological and pathophysiological implications and recommendations for physical and nutritional countermeasures
Marco Naricia, Giuseppe De Vitoa, Martino Franchib, Antonio Paolic, Tatiana Moroc, GiuseppeMarcolinc, Bruno Grassid, Giovanni Baldassarred, Lucrezia Zuccarellid, Gianni Bioloe, Filippo Giorgio di Girolamoe, Nicola Fiottie, Flemming Delaf,g, Paul Greenhaffh, and ConstantinosMaganarisi
a Department of Biomedical Sciences, CIR-MYO Myology Center, Neuromuscular Physiology Laboratory, University of Padova, Padua, Italy
b Department of Biomedical Sciences, Neuromuscular Physiology Laboratory, University of Padova, Padua, Italy
c Department of Biomedical Sciences, Nutrition and Exercise Physiology Laboratory, University of Padova, Padua, Italy
d Department of Medicine, University of Udine, Udine, Italy
e Department of Internal Medicine, University of Trieste, Ospedale di Cattinara, Trieste, Italy
f Xlab, Department of Biomedical Sciences, University of Copenhagen, Copenhagen, Denmark
g Department of Geriatrics, Bispebjerg-Frederiksberg University Hospital, Copenhagen, Denmark
hMRC Versus Arthritis Centre for Musculoskeletal Ageing Research, Centre for Sport, Exercise and Osteoarthritis Research Versus Arthritis, National Institute for Health Research Nottingham Biomedical Research Centre, School of Life Sciences, The Medical School, University of Nottingham, Queen's Medical Centre, Nottingham, UK
i School of Sport and Exercise Sciences, Liverpool John Moores University, Liverpool, UK
ABSTRACT
The COVID-19 pandemic is an unprecedented health crisis as entire populations have been asked to self-isolate and live in home-confinement for several weeks to months, which in itself represents a physiological challenge with significant health risks. This paper describes the impact of sedentarism on the human body at the level of the muscular, cardiovascular, metabolic, endocrine and nervous systems and is based on evidence from several models of inactivity, including bed rest, unilateral limb suspension, and step-reduction. Data form these studies show that muscle wasting occurs rapidly, being detectable within two days of inactivity. This loss of muscle mass is associated with fibre denervation, neuromuscular junction damage and upregulation of protein breakdown, but is mostly explained by the suppression of muscle protein synthesis. Inactivity also affects glucose homeostasis as just few days of step reduction or bed rest, reduce insulin sensitivity, principally in muscle. Additionally, aerobic capacity is impaired at all levels of the O2 cascade, from the cardiovascular system, including peripheral circulation, to skeletal muscle oxidative function. Positive energy balance during physical inactivity is associated with fat deposition, associated with systemic inflammation and activation of antioxidant defences, exacerbating muscle loss. Importantly, these deleterious effects of inactivity can be diminished by routine exercise practice, but the exercise dose–response relationship is currently unknown. Nevertheless, low to medium-intensity high volume resistive exercise, easily implementable in home-settings, will have positive effects, particularly if combined with a 15–25% reduction in daily energy intake. This combined regimen seems ideal for preserving neuromuscular, metabolic and cardiovascular health.
Highlights•This paper describes the impact of sedentarism, caused by the COVID-19 home confinement on the neuromuscular, cardiovascular, metabolic and endocrine systems.•Just few days of sedentary lifestyle are sufficient to induce muscle loss, neuromuscular junction damage and fibre denervation, insulin resistance, decreased aerobic capacity, fat deposition and low-grade systemic inflammation.•Regular low/medium intensity high volume exercise, together with a 15-25% reduction in caloric intake are recommended for preserving neuromuscular, cardiovascular, metabolic and endocrine health.
KEYWORDS
COVID-19, sedentarism, neuromuscular system, cardiovascular system, glucose homeostasis, body composition, nutrition, exercise
CONTACT Correspondence: Marco Narici. E-mail: marco.narici@unipd.it
© 2020 European College of Sport Science
Introduction
The COVID-19 pandemic is posing a very serious challenge to our societies as entire populations have been asked to restrict their social interactions and in many countries even to self-isolate and live in home-confinement for several weeks to months. This period of restricted movement affects all citizens regardless of age, sex and ethnicity. It forces people, even the youngest and fittest, to become suddenly inactive and adopt sedentary behaviours.
This short position-point paper aims to explain the impact of sedentarism on the human body at the level of the muscular, cardiovascular, metabolic, endocrine and nervous systems and is based on knowledge derived from several models of inactivity, including bed rest, unilateral limb suspension, and step-reduction. Evidence is provided on the degree and speed of muscle atrophy we can expect when undergoing a period of complete inactivity caused by bed rest. Notably, muscle atrophy is a very fast phenomenon detectable after just two days of inactivity. The novel and concerning findings of muscle denervation and damage to the neuromuscular junction associated with inactivity are also discussed. The mechanisms of disuse muscle atrophy are also examined in terms of muscle protein metabolism and cellular signalling, highlighting the different temporal contributions of changes in muscle protein synthesis and degradation and how these processes differ between young and older populations and can impact on muscle mass restoration during recovery. Additionally the concept of anabolic resistance, in the context of inactivity and ageing, and its role in impairing the anabolic response to feeding and exercise is considered. This paper also critically addresses the impact of bed rest and of step-reduction on glucose metabolism and on the pivotal role of skeletal muscle in inactivity-induced insulin resistance. Evidence is provided that inactivity leads to a specific reduction in muscle insulin sensitivity without affecting that of the liver. The noteworthy observations that just few days of step-reduction can induce insulin resistance and that changes in insulin sensitivity precede muscle atrophy and changes in body composition are also brought to the reader’s attention. Bed-rest and step reduction also have a major impact on aerobic capacity, yielding remarkably similar losses in VO2max within two weeks of inactivity (bed rest)/reduced activity (∼7%). It is also noteworthy that the impairment of VO2max after this period of inactivity is twice as large in older (aged 60 years) compared to younger individuals. A decrease in VO2max is associated with an increased mortality rate. Fundamentally, the available data shows that few days/weeks of inactivity impair the O2 pathway at all levels, from the cardiovascular system, including peripheral circulation, to the oxidative function of skeletal muscles. This paper also examines the relevance of nutritional intake versus energy expenditure on lean muscle loss, body fat and systemic inflammation. In particular, the observations that excess fat deposition during physical inactivity is associated with greater muscle loss and greater activation of systemic inflammation and antioxidant defences are highlighted. The contribution of these mechanisms to long-term changes in body composition and to the development of cardiometabolic risk in healthy sedentary persons are also explained. The importance of reducing caloric intake to match the energy expenditure is emphasised in this paper, and recommendations are given for maintaining a normal number of meals/day per day, without snacking and with a long overnight fast. The role of fasting on inflammation and on the immune response are also addressed.
Finally, this paper provides recommendations for lifestyle, exercise and nutritional interventions to prevent loss of muscle mass, aerobic capacity, insulin sensitivity and of neuromuscular integrity during long periods of home-confinement, and also to increase muscle mass restoration following prolonged periods of inactivity or immobilisation.
Impact of inactivity on the neuromuscular system and the protective action of exercise: don’t stop the music, your muscles are still listening!
The negative consequences of inactivity on the muscular system have long been recognised since the early 20’s by Cuthbertson (1929) who suggested that prolonged rest in healthy subjects leads to a loss of nitrogen, phosphorous and calcium due to non-use of muscles and bones. Forty years later, Saltin et al. (1968), a pioneer in human applied physiology, showed that in response to 20-day bed confinement, young healthy individuals lose on average 28% of maximum oxygen uptake (VO2max) and 11% of heart volume.
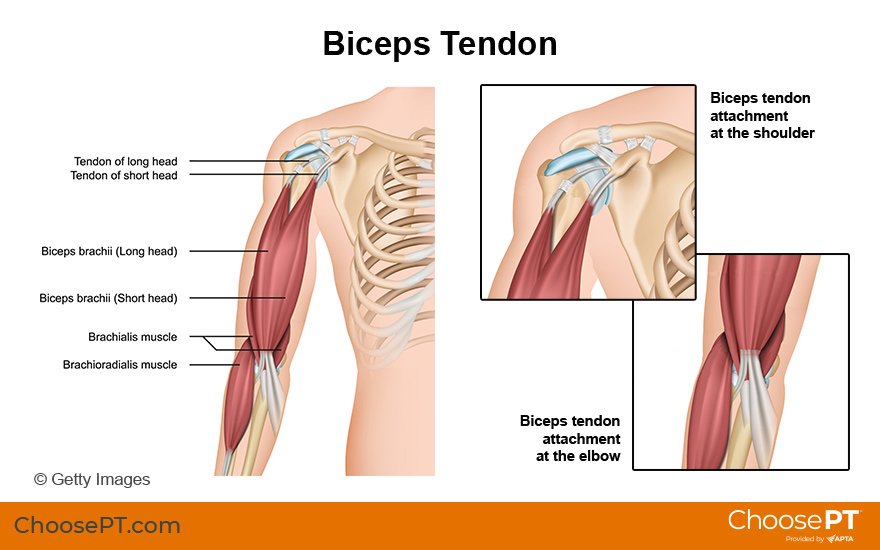
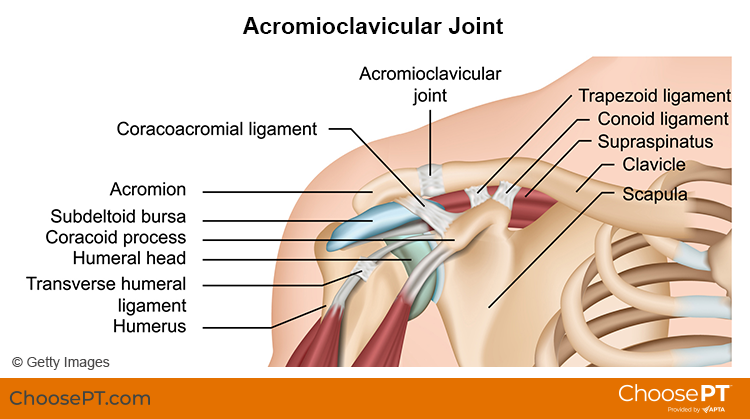
It is now firmly established that inactivity, induced by bed rest, limb casting, limb suspension or by simple sedentarism, causes a rapid loss of muscle mass, particularly of the antigravity muscles that are constantly used for sustaining an upright posture, to perform movement and for maintaining balance. The resulting loss of muscle function affects both muscle strength and power and it is noteworthy that the loss of muscle function typically exceeds that of muscle size, indicating that muscle with disuse becomes intrinsically weaker. Atrophy and loss of contractile force and force per unit cross-sectional area are also found at single fibre level, together with a gradual shift in myosin isoforms towards the fast type. Recent evidence shows that inactivity also causes damage to the neuromuscular junction and muscle denervation (Narici et al., 2020), which suggest that muscle atrophy not only arises from the reduction in mechanical loading but also from neurodegenerative processes. The significant deterioration of the muscular system caused by inactivity emphasises the fundamental importance of exercise for preserving muscle mass and neuromuscular function when unexpected conditions, such as the latest COVID-19 outbreak, cause a drastic restriction of daily movement compared to habitual life.
The impact of sedentarism on muscle mass
A recent survey performed on the impact of sedentarism on 6733 people aged 18–98 years showed a clear association between low physical activity or age, and fat-free mass and body fat, normalised to body height (Kyle, Morabia, Schutz, & Pichard, 2004). Essentially, the study demonstrated that physical activity was successful for maintaining fat-free mass, prevented excess body fat and resulted in lower rates of obesity. Also, when comparing muscle mass and muscle power of sedentary people aged 20–80 years to those of a population of age-matched master power athletes, it is clear that maintaining a high physical activity level preserves muscle mass and power throughout the lifespan (Grassi, Cerretelli, Narici, & Marconi, 1991). This benefit translates into a gain of 20–25 years in terms of biological age when muscle mass and performance of master athletes and sedentary peers and of master weightlifters and active older peers are compared (Grassi et al., 1991; Pearson et al., 2002). Similarly, lifelong trained individuals show 30% greater muscle strength compared to age-matched sedentary people (Aagaard, Magnusson, Larsson, Kjaer, & Krustrup, 2007). Remarkably, the benefits conferred by an active lifestyle protect not only against the loss of muscle mass and strength but also seem to protect against the progressive muscle denervation that accompanies the ageing process and is exacerbated by inactivity. In fact, when comparing muscle biopsies of older sedentary people with those of seniors with a long history of high-level recreational sport activities, significantly fewer denervated fibres are found in the life-long athletes (Mosole et al., 2014).
Lessons from prolonged bed-rest and unloading studies in man
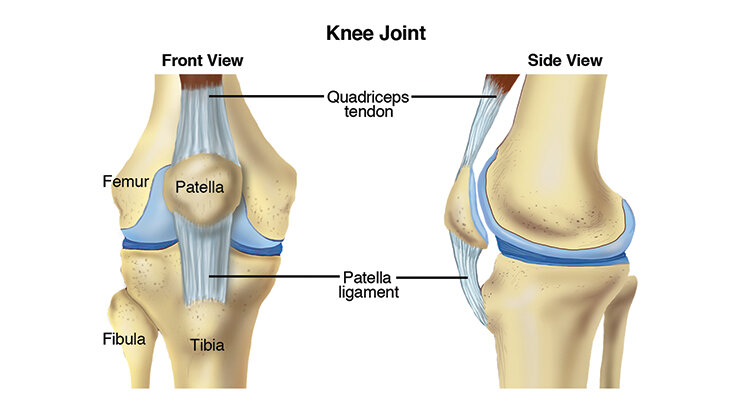
Preservation of muscle mass requires a constant supply of mechanical stimuli that stimulate directly, or indirectly protein synthesis. When we stop loading our muscles, these essential stimuli required for muscle anabolism are removed (see Sect. Physical inactivity and the regulation of muscle mass) and the balance between protein synthesis and protein degradation tips towards degradation. Within a few days, objective signs of muscle atrophy can be found. Indeed, significant quadriceps atrophy is found after just 2 days of leg immobilisation (1.7%) (Kilroe, Fulford, Jackman, Van Loon, & Wall, 2020), 3 days of dry-immersion (2%) (Demangel et al., 2017) or 5 days bed rest (2%) (Mulder et al., 2015), associated with an even greater loss of muscle strength (8–9%) (de Boer, Maganaris, Seynnes, Rennie, & Narici, 2007; Demangel et al., 2017; Mulder et al., 2015). Over the following days and weeks, quadriceps atrophy progresses at an inexorable pace, 6% ca. after 10 days (Narici et al., 2020), 10% after 29 days (Alkner & Tesch, 2004a), 13% after 60 days (Mulder et al., 2015), reaching 18% after 90 days (Alkner & Tesch, 2004b). This rate of muscle atrophy follows an exponential time course, predicting a ∼10% loss of muscle mass in 30 days and ∼15% in 60 days. Similar results are found in other disuse paradigms, such as in unilateral lower limb suspension (ULLS). The lack of use of one lower limb for 3 weeks results in 5% muscle loss after 10 days and 10% after 21 days of ULLS (de Boer, Maganaris, et al., 2007).
Hence it is clear that complete inactivity of the entire body, or segments of it, will lead to an unavoidable and predictable muscle loss.
Inactivity also compromises muscle innervation and nerve-muscle cross-talk
Up to recent times, it was assumed that muscle loss caused by inactivity was simply due to the lack of mechanical loading of muscles. However, there is now increasing evidence that chronic inactivity, caused by bed rest for example, triggers muscle fibre denervation and damage to the neuromuscular junction (NMJ). In humans, the presence of muscle denervation may be demonstrated by measuring neural cell adhesion molecule (NCAM)-positive muscle fibres. NCAM is a glycoprotein normally expressed during embryonic development but absent in adult muscle; hence, its presence in adult muscle is indicative of an ongoing denervation/reinnervation process, as seen in paralysis or in other neurodegenerative disease conditions (Dickson et al., 1987). Indeed, an increase in NCAM positive muscle fibres has been found in three separate bed rest studies lasting 3, 10 and 15 days, respectively (Arentson-Lantz, English, Paddon-Jones, & Fry, 2016; Demangel et al., 2017; Narici et al., 2020). Also, inactivity leads to damage to the NMJ. A decreased expression of Homer protein, a component of the NMJ involved in translating of neuromuscular synaptic input to the calcineurin-NFAT signalling cascade in skeletal muscle fibres, has been found after 60-day bed rest (Salanova et al., 2011). Similarly, increased levels of c-terminal Agrin fragment, a serum marker of NMJ damage (Hettwer et al., 2013), have been recently found after 10 days of bed rest (Narici et al., 2020). Collectively, these findings provide evidence that chronic inactivity triggers neurodegenerative processes inducing muscle denervation and NMJ damage. The speed with which these changes occur emphasise even more the essentiality of exercise as not only muscle, but also innervation and muscle-nerve cross-talk, are compromised by periods of chronic inactivity.
Exercise for neuromuscular health
The evidence that exercise is of vital importance for preserving the integrity and function of the neuromuscular system is incontrovertible. Numerous studies have shown that when resistive exercise, in various forms, is applied during bed rest periods, the loss of muscle mass is significantly mitigated or fully prevented (Alkner & Tesch, 2014a, 2014b; Belavý, Miokovic, Armbrecht, Rittweger, & Felsenberg, 2009; Kawakami et al., 2001). Likewise, the comparison of neuromuscular decline in sedentary versus active seniors, confirms the essential role of exercise for the prevention of neuromuscular system impairment with inactivity. When dealing with inactivity, or reduced activity, the essential goal of any exercise countermeasure programme should be to preserve normal physiological function. In this respect, we should provide our muscular system with loading activities (intensity and duration) similar to those encountered during habitual, unrestricted, ambulatory activities. In so doing we would also “keep in tune” motoneurons and motor end-plates, ensuring uncompromised nerve-muscle cross-talk. As motoneurons are particularly rich in mitochondria, regular physical activity, particularly if aerobic in nature, seems essential for preventing mitochondrial dysfunction and oxidative damage to the motoneuron and the NMJ. Also, exercise is known to maintain neurotrophin release, whose action plays an essential role in maintaining neuromuscular system integrity (Nishimune, Stanford, & Mori, 2014).
Thus to achieve protection of the neuromuscular system, exercise should involve both high intensity resistive exercises for preserving muscle mass as well as aerobic exercise for preserving neuromuscular system integrity and mitochondrial function (see Sect. Physical inactivity and the cardiorespiratory system). Performing high-intensity resistive exercises typically requires the use of weights and specialised machines, such as those found in gyms. However, experimental evidence shows that exercising with slow contractions at a relatively low intensity, about ∼50% of 1 RM (3 s concentric and 3 s eccentric contraction with no rest in between), produces the same gains in muscle size as training at ∼80% of the 1RM (1 s concentric, 1 s eccentric, 1 s rest) (Tanimoto & Ishii, 2006). Performing such lower intensity contractions is possible in home-settings without any specialised equipment or machines, e.g., by bodyweight exercises and resistance elastic bands. It thus seems likely that preserving muscle mass can be achieved at home, without access to classical weight training or sophisticated equipment. It is also noteworthy that training with low loads high volume contractions (30% 1RM, 24 repetitions), has been found to lead to a greater increase in protein synthesis than training with high-load, low volume (90% 1RM, 5 repetitions) contractions (Burd et al., 2010). Hence low to medium-intensity high volume resistive exercise seem particularly effective for preserving, or most likely developing, muscle mass. This seems particularly relevant for the present home-confinement period, in which training with high loads is not feasible and does not seem anyway to produce a greater anabolic response.
As for the aerobic exercise, any workouts involving repeated exercises with large muscle groups such as rope-skipping, jogging in place, burpees, mountain climbers, seem suitable. These exercises could take the form of a circuit training where aerobic exercises are alternated with resistive ones trying to complete a fixed set of repetitions in rapid succession. The intensity and the volume could be manipulated by increasing either the number of repetitions/circuits completed or the speed of execution. This form of training can have many advantages such as reduced monotony, improvements in both aerobic capacity and muscle strength, and ultimately overall health (Muñoz-Martínez, Rubio-Arias, Ramos-Campo, & Alcaraz, 2017).
An extremely effective workout, particularly suited for a young and fit population, is full body high intensity interval training (HIIT). Home-based HIIT workouts do not require any equipment and provide rapid improvements in terms of muscle power, cardiorespiratory fitness and glucose metabolism (Blackwell et al., 2017; Karlsen, Aamot, Haykowsky, & Rognmo, 2017).
Hence, when facing period of restricted activity due to home confinement as in the present COVID-19 pandemic, the main recommendation for preserving neuromuscular health is to exercise daily with slow, low/medium-intensity high volume contractions and to perform aerobic exercise workouts involving large muscle groups. Remember that exercise is music for your muscles, don’t stop playing as they are still listening!
Physical inactivity and the regulation of muscle mass: you keep on moving
A number of factors are reported to increase risk for poor metabolic health and functional decline, including mental disorders, physical disabilities, physical inactivity and sedentary time (time spent sitting). Of these, physical inactivity and time spent sitting appear to be the most prevalent risk factors (de Rezende, Rey-López, Matsudo, & do Carmo Luiz, 2014; Matthews et al., 2012; Wilmot et al., 2012), but unfortunately most individuals are currently unaware of the potential insidious health risks associated with not moving. Time spent sitting has been linked with increased risk of all-cause mortality (Katzmarzyk, Church, Craig, & Bouchard, 2009), cause specific mortality (Katzmarzyk et al., 2009; Wilmot et al., 2012), cardiovascular disease (Stamatakis, Hamer, & Dunstan, 2011) and poor metabolic health (Ford et al., 2010; Hu, Li, Colditz, Willett, & Manson, 2003). A large scale (3720 men and 1412 women) 16-year follow-up study, in which a total of 450 deaths was recorded, however reported no clear associations between any of 5 different indicators of sitting time with mortality risk, and pointed to physical inactivity per se as the central driver of mortality risk (Pulsford, Stamatakis, Britton, Brunner, & Hillsdon, 2015). It is therefore of genuine concern that physical inactivity and sedentary behaviours are likely to be common place during the current coronavirus (COVID-19) pandemic. Moreover, it is vital to raise awareness of the associated health risks. This section will focus on the impact of inactivity on the regulation of muscle mass and what we understand about maintaining muscle mass during and after such physiological insult. Please be aware that inactivity is indeed a physiological insult, and its effects manifest very quickly.
Immobilisation studies
The maintenance of muscle mass is dependent on the balance between rates of muscle protein synthesis and muscle protein breakdown, where a chronic imbalance results in either the loss or gain of muscle mass. Much insight regarding the regulation of muscle mass in humans during inactivity has been gleaned from bed-rest or single limb immobilisation (casting) studies. From such studies it is generally agreed that immobilisation induced suppression of muscle protein synthesis is the primary driver of muscle mass loss in humans. For example, de Boer, Selby, et al., (2007) detected a 50% decline in the rate of post-absorptive myofibrillar protein synthesis measured over several hours following 10 days of limb suspension in healthy, young volunteers when compared to baseline. The authors concluded that the immobilisation induced suppression of muscle protein synthesis was of sufficient magnitude to fully account for the loss of muscle cross sectional area recorded, i.e. the contribution from muscle protein breakdown to total muscle mass loss during immobilisation was small (de Boer, Selby, et al., 2007). It is important to recognise, however, this does not preclude a role for muscle protein breakdown during immobilisation in humans. Indeed, increased amounts of markers of muscle protein breakdown, such as ubiquitin protein conjugates (Abadi et al., 2009) and increased 3-methylhistidine release (Tesch, von Walden, Gustafsson, Linnehan, & Trappe, 2008), have been observed in the first few days of muscle disuse in volunteers pointing to an early and possibly transient contribution of muscle protein breakdown to muscle mass loss. Of further health importance, despite a clear appreciation of the importance of muscle mass to longevity with ageing (Srikanthan & Karlamangla, 2014), some authors have reported three-fold greater muscle mass loss during immobilisation in older compared to young people (Paddon-Jones et al., 2006), whilst others report the diametric opposite (Suetta et al., 2009). In short, we do not yet fully understand the interaction between muscle ageing processes and immobilisation induced muscle mass loss.
Reduced step count studies
In the limited number of studies where semi-quantitative approaches have been used to control physical activity levels, reduced levels of physical activity (from 10,500–1300 steps/day for 2 weeks) induced muscle insulin resistance and the loss of lean leg mass in young males (Krogh-Madsen et al., 2010). Further evidence reports that 2 weeks of reduced physical activity (from >3500 to <1500 steps/day) in healthy older people (>65 years and normally the most inactive proportion of the population) induced a small but measurable increase in whole-body insulin resistance and blunted post-prandial rates of muscle protein synthesis (Breen et al., 2013). Rather alarmingly, severe reductions in daily step counts to far below the recommendation of remaining >5000 steps per day to avoid sedentarism, such as that seen in hospitalised older women (>65 years, n = 239) with an acute medical illness where ambulatory activity was found to be on average 740 steps/day (interquartile range 89–1014 steps/day) (Fisher et al., 2011), can initiate a downward spiral resulting in severe deconditioning and long-lasting functional deficits (Hirsch, Sommers, Olsen, Mullen, & Winograd, 1990). Importantly, what is astonishing is that the time-course of inactivity induced metabolic dysfunction appears to be far quicker than the positive impact of increasing physical activity levels. For example, a 2 week transition period from an ambulatory lifestyle (without structured exercise training) to inactivity, induces insulin resistance, increases central adiposity and reduces muscle mass in healthy, young volunteers (Thyfault & Krogh-Madsen, 2011), whilst restoration of metabolic function and muscle volume, particularly following marked inactivity such as immobilisation, can take longer than might be expected, especially in older people. For example, 4 weeks of supervised strength training involving three sessions each week did not restore muscle volume following only 2 weeks of immobilisation in older males (Suetta et al., 2009). This is clearly of significant concern in the current circumstances of social distancing and isolation that is likely to continue for several months, and moreover where metabolic and physiological fitness appear to be associated with disease susceptibility.
Cellular and molecular mechanisms controlling inactivity induced muscle mass loss
Research has highlighted protein translation initiation, where the ribosomal structure is formed and the associated mRNA transcript becomes bound in response to increased dietary protein intake and/or muscle contraction, as a key point of regulation of muscle protein synthesis. The Akt/mTOR/p70S6K signalling cascade has been assigned a central role in this nutrient and/or contraction mediated activation of protein translation initiation, and is founded on elegant experiments demonstrating high frequency electrical stimulation of rodent muscle occurs in parallel with increased phosphorylation of these signalling proteins (Atherton et al., 2005) and muscle specific over-expression of Akt in transgenic mice results in muscle hypertrophy (Bodine et al., 2001). However, accumulating evidence suggests that the Akt/mTOR/p70S6K signalling cascade has no obvious role in the regulation of the decline in muscle protein synthesis seen during immobilisation, given neither the phosphorylation state nor content of Akt, p70S6K, 4E-BP1 or eIF4E were altered in the post-absorptive state following 10 or 21 days of limb suspension (de Boer, Selby, et al., 2007). Furthermore, although immobilisation blunted the increase in muscle protein synthesis in response to increased amino acid availability (so called anabolic blunting) in healthy volunteers when compared to a non-immobilised contralateral limb (even under conditions of high amino acid provision), this anabolic blunting occurred in the face of similar changes in the phosphorylation state of the Akt/mTOR/p70S6K signalling pathway in both limbs (Glover et al., 2008). Collectively these findings from volunteer studies highlight that Akt/mTOR/p70S6K signalling pathway is unlikely to be regulating the deficits in post-absorptive or post-prandial muscle protein synthesis observed during immobilisation in humans. On balance, it would seem the precise mechanisms responsible for the decline in muscle mass observed during immobilisation in humans remain to be elucidated.
You can’t always get what you want: but if you try sometimes you might just find you get what you need
On a positive note, interventional research trials have indicated that intermittent walking breaks during prolonged periods of sitting can improve indices of metabolic health (Dunstan et al., 2012; Healy et al., 2008), and that reducing sedentary behaviour has measurable positive effect on cardio-metabolic health that can be differentiated from exercise training (Macfarlane, Taylor, & Cuddihy, 2006). From the perspective of the maintenance of muscle mass, we do not yet know the precise relationship between exercise dose (daily frequency and intensity) and muscle mass retention during prolonged periods of immobilisation or inactivity. However, it is known that resistance exercise will be an effective intervention. For example, it has been shown that undertaking resistance exercise during 60 days bed rest maintained, and increased, the cross-sectional area of the soleus and vastus lateralis leg muscles, respectively (Trappe, Creer, Slivka, Minchev, & Trappe, 2007). It also prevented decrements in type I and IIa fibre diameters, maintained the proportion of hybrid fibres (Trappe et al., 2007), and prevented increases in markers of muscle protein breakdown (Salanova, Schiffl, Püttmann, Schoser, & Blottner, 2008). Such findings highlight the effectiveness of resistance exercise countermeasures to prevent muscle atrophy. Furthermore, observations of greater calf muscle cross sectional area compared to baseline in subjects 3, 6 and 12 months after 90 days bedrest (Rittweger & Felsenberg, 2009) highlights the enormous plasticity of the muscle to exercise intervention following prolonged immobilisation, at least in young people. Indeed, most of the exercise induced restoration of calf muscle volume occurred in the first phase of recovery in this study (Rittweger & Felsenberg, 2009), pointing to growth rates not being directly proportional to the magnitude of the exercise stimulus, i.e. muscle is more sensitised to grow in the early period following immobilisation induced atrophy (although it is not clear why). These studies highlight the effectiveness of muscle contraction as a countermeasure to prevent muscle loss during immobilisation and inactivity in young volunteers, and also to increase muscle mass restoration following prolonged periods of inactivity or immobilisation (but maybe less so in older people; Suetta et al., 2009). Importantly, the molecular mechanisms by which exercise exerts such positive effect(s) remain unknown, but such insight would greatly help our understanding of how to maintain muscle mass and metabolic health in any future public health crisis requiring social distancing and isolation.
Physical inactivity and glucose homeostasis
In the present coronavirus disease (COVID-19) pandemic, millions of people world-wide are being confined to little social activity and stay-at-home restrictions. This means that for almost every individual the level of daily physical activity will be reduced considerably and very quickly. We have well-documented information on the importance of being physically active to maintain health, and therefore the present situation of markedly reduced physical activity to levels well below the daily recommendation of 7500–10,000 steps per day will exacerbate health problems arising from physical inactivity (Blair, 2009; Booth, Roberts, Thyfault, Rugsegger, & Toedebusch, 2017). Indeed, unfavorable indicators of body composition and cardiometabolic risk have been consistently associated with taking <5000 steps/day. Importantly, negative health effects can be seen relatively quickly (3–14 days) when the transition is marked, e.g. from >10,000 to less than 5000 or as low as 1500 daily step counts (Tudor-Locke, Craig, Thyfault, & Spence, 2013), as will be happening around the world in the current pandemic.
This section will cover the consequences of inactivity on glucose homeostasis and provide advice on simple measures to offset the negative effects of physical inactivity. The first study demonstrating the deleterious effect of physical inactivity on glucose tolerance was published 75 years ago in patients confined to bed for various length of time, such as patients with hip or femoral fractures, multiple sclerosis, hemiplegia, coxa vara etc. (Blotner, 1945). It is now well established that sedentary activities such as desk work, TV viewing, sitting (Dunstan et al., 2005; Katzmarzyk et al., 2009; Van der Ploeg, Chey, Korda, Banks, & Bauman, 2012) are associated with increased all-cause mortality and increased morbidity (metabolic syndrome, cardiovascular disease). The association is summarised in a recent review that concluded: “Higher levels of total physical activity, at any intensity, and less time spent sedentary are associated with a substantially reduced risk for premature mortality, with evidence of a non-linear dose–response pattern in middle aged and older adults” (Ekelund et al., 2019).
Bed-rest studies
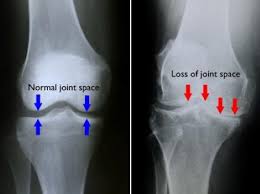
Structured intervention studies with advanced end-point measurements have been carried out in healthy volunteers confined to strict bed-rest. Such studies with 7–10 days bed-rest in healthy individuals (Mikines, Richter, Dela, & Galbo, 1991; Sonne et al., 2010; Stuart, Shangraw, Prince, Peters, & Wolfe, 1988) have shown that immobilisation leads to a 10–34% decrease whole body insulin sensitivity (measured by the hyperinsulinemic, glucose clamp technique). However, the decrease of insulin sensitivity measured by the arterio-venous balance technique in the forearm (Sonne et al., 2010; Stuart et al., 1988) or the leg (Mikines et al., 1991), was much greater, 47–75%. Metabolically speaking, the forearm and the leg consist of predominantly skeletal muscle, emphasising the pivotal role of skeletal muscle in inactivity induced insulin resistance, which appears to be attributable to the reduction in muscle contraction per se (Crossland, Skirrow, Puthucheary, Constantin-Teodosiu, & Greenhaff, 2019). The central role of skeletal muscle in inactivity induced insulin resistance is also highlighted by the fact that hepatic insulin sensitivity is not affected by short-term bed rest (Mikines et al., 1991; Stuart et al., 1988).
Therefore, the mechanisms behind the inactivity induced decrease in whole-body insulin sensitivity and impaired glucose tolerance (Alibegovic et al., 1988; Arciero, Smith, & Calles-Escandon, 1998; Dolkas & Greenleaf, 1977; Hamburg et al., 2007; Knudsen et al., 2012; Krogh-Madsen et al., 2010; Lipman, Schnure, Bradley, & Lecocq, 1970; Mikines et al., 1991; Myllynen, Koivisto, & Nikkila, 1987; Richter, Kiens, Mizuno, & Strange, 1989; Rogers, King, Hagberg, Ehsani, & Holloszy, 1990; Sonne et al., 2010; Sonne et al., 2011; Stuart et al., 1988; Vukovich et al., 1996) are coupled to changes within the skeletal muscle. The decrease in skeletal muscle insulin sensitivity with physical inactivity is not linked to changes in body composition (loss of muscle mass, increase in body fat percentage) (Knudsen et al., 2012) as the insulin resistance develops rapidly (within a few days) and long before muscle atrophy and increases in body fat (or ectopic fat deposition) sets in.
In contrast, there is a reduction in skeletal muscle metabolic capacity with inactivity. GLUT4 transporter protein content and glycogen synthase activation decreases (Bienso et al., 2012; Op’t, Urso, Richter, Greenhaff, & Hespel, 2001; Tabata et al., 1999; Vukovich et al., 1996) as well as mitochondrial DNA content, hexokinase II and sirtuin 1 protein content (Ringholm et al., 2011). Also insulin-induced Akt phosphorylation and 3-hydroxyacyl-CoA dehydrogenase (HAD) activity have been found to decrease in some (Bienso et al., 2012; Krogh-Madsen et al., 2010; Ringholm et al., 2011), but not all (Mikines et al., 1991; Mortensen et al., 2014) bed-rest studies. Muscle capillary density does not change with short-term bed-rest (∼7 days) (Mikines et al., 1991; Ringholm et al., 2011), but microvascular dysfunction will develop (Hamburg et al., 2007; Sonne et al., 2010; Sonne et al., 2011). Of note, after 7-day bed-rest the normal exercise induced response of AMP-activated protein kinase phosphorylation, peroxisome proliferator activated receptor- coactivator-1, and VEGF mRNA content in skeletal muscle is abolished (Ringholm et al., 2011), underlining the profound effect of physical inactivity on muscle metabolism.
On the gene expression level, it has been found that 9 days of bed-rest altered the expression of ∼4500 genes, with downregulation of 34 pathways, mostly associated with mitochondrial function (PPARγ coactivator-1α, NADH dehydrogenase 1 β-subcomplex 6) and insulin resistance (e.g. hexokinase II, ras-related associated with diabetes (RRAD)) (Alibegovic et al., 2010). Notably, these genes reversed to pre- bed-rest levels after 4 wks of re-training (Alibegovic et al., 2010).
Parallel to, and possibly linked with inactivity induced insulin resistance, is the elevated inflammatory burden which may occur with prolonged bed rest (Crossland et al., 2019; Kwon et al., 2015). However, not all studies have found that skeletal muscle inflammation plays a role in short-term bed rest induced insulin resistance (Friedrichsen et al., 2012).
Studies with reduced ambulatory activity
Strict bed-rest is a drastic model, which may not comply with the situation for most people affected by the COVID-19 restrictions, but just reducing daily physical activity has a negative impact on glucose homeostasis. There are many observational studies demonstrating this, but only a few interventional studies. By employing accelerometer controlled reductions in daily step counts from ∼10,000–12,000/day to ∼1000 steps/day, two studies showed that glycemic control and indices of insulin sensitivity markedly deteriorated already after 3 days of daily step reductions (Knudsen et al., 2012; Mikus et al., 2012) in young healthy men. After a total of 14 days of step count reduction, insulin sensitivity was decreased by 17–44% (Knudsen et al., 2012; Krogh-Madsen et al., 2010). Notably, hepatic insulin sensitivity did not change (Krogh-Madsen et al., 2010), again underscoring the important role of skeletal muscle. In older (∼69 years) pre-diabetic people, the same negative effect of reducing daily steps for 2 weeks is seen, but even worse, glycaemic control did not recover after additional 2 weeks with return to normal physical activity (McGlory et al., 2018).
Measures to offset the negative effects of physical inactivity
How low can you go? At the present time we do not know the exercise dose or frequency required to offer protection from inactivity. Exact thresholds for specific minimal physical activity is not possible to define accurately, but measurements of daily steps (measured by pedometers or accelerometers) have provided useful insight. Less than 5000 steps per day seems to be associated with unfavourable indicators of body composition, cardiometabolic risk, insulin sensitivity and glycemic control (Tudor-Locke et al., 2013). For this reason <5000 steps/day has been proposed as the threshold defining a sedentary lifestyle for adults (Tudor-Locke et al., 2013). Fundamentally, the aim must be to increase energy expenditure through muscular work, as light as it may be. Simple measures, such as alternating between sitting and standing for 30 min periods during desk-top work, will result in a small, but meaningfully and significant increase in energy expenditure (Gibbs, Kowalsky, Perdomo, Grier, & Jakicic, 2017).
Intervention studies involving interruption of sitting time with standing (Benatti et al., 2017) or light-intensity walking (Pulsford, Blackwell, Hillsdon, & Kos, 2017) have been carried out in healthy males, aged ∼30 and ∼40 years of age, respectively. One study found that breaking up prolonged sitting with non-ambulatory standing during 9 h, acutely reduced post-prandial glycemic response (Benatti et al., 2017), while another study found the opposite, namely that during 8.5 h interrupting sustained sitting with brief repeated bouts of light-intensity walking but not standing improved glycemic control (Pulsford et al., 2017). Similar experiments have been done over four days in patients with type 2 diabetes, in whom the importance for daily physical activity is even greater. The authors compared breaking up sitting ∼14 h/day with either structured ergometer exercise for ∼1 h or breaking up sitting every half hour with standing (in total 3 h) and light intensity walking (in total 2 h) (Duvivier et al., 2017). The “Sit Less” (interrupting sitting with standing/walking) was superior to structured exercise in terms of glycemic control (Duvivier et al., 2017); a conclusion that was also reached in healthy young individuals with a comparable intervention (Duvivier et al., 2013). Furthermore, the findings in patients with type 2 diabetes (Duvivier et al., 2017) is supported by an earlier study in patients with type 2 diabetes showing that 3 × 10 min exercise per day is preferable to 1 × 30 min per day (Eriksen, Dahl-Petersen, Haugaard, & Dela, 2007).
The cellular mechanisms linking physical inactivity and/or sedentary time to impaired metabolic health are not known in details. Only pieces of information are available, as described above. Unfortunately, most individuals are currently unaware/and or unconvinced of the potential insidious health risks associated with prolonged periods of inactivity and/or sitting. What is also remarkable is that the time-course of inactivity induced metabolic dysfunction appears to be far quicker than the positive impact of increasing physical activity levels. In the times of restrictions due to the COVID16 pandemic it is important to realise that a modest amount of moderate-intensity daily exercise (equivalent to 30 min per day) is necessary (Slentz, Houmard, & Kraus, 2007). Any addition to this minimal regimen will lead to improvements in many health measures. In the words of the Rolling Stones “You Gotta Move”!
Physical inactivity and the cardiorespiratory system: a matter of survival
A study carried out a few years ago by Prof. Bente Pedersen’s group (Krogh-Madsen et al., 2010) anticipated the condition to which hundreds of millions of people, around the world, are now exposed as a consequence of the home confinement in response to the COVID-19 pandemic: a drastic reduction in the level of physical activity. In that study (Krogh-Madsen et al., 2010) a group of healthy young males acutely reduced the number of steps per day, from a baseline of ∼10,000 to ∼1350, and maintained this lower level of activity for 2 weeks. To put this value into the right context: (i) a number of steps/day lower than ∼5000 identifies a “sedentary life-style” (Slentz et al., 2007); (ii) a threshold of ∼4500–6000 steps/day is considered the minimum necessary to avoid an increased cardio-metabolic risk (1); and (iii) ∼10,000 steps/day represents a reasonable target for healthy adults (Slentz et al., 2007). After the 2 weeks of reduced activity the subjects presented a ∼7% decrease in maximal O2uptake (, taken as an index of “cardiorespiratory fitness”), a ∼3% decrease in lean leg mass and a decreased insulin sensitivity (Krogh-Madsen et al., 2010). The parallel decreases of , leg lean mass and insulin sensitivity were considered clinically relevant, since all three factors independently increase mortality.
Decrease in and impairment of O2 transport and utilisation mechanisms
Interestingly, the rate of decrease in described in the study by Krogh-Madsen et al. (2010), that is ∼7% over 2 weeks, corresponding to a rate of decrease of ∼0.5%/day, was remarkably similar to the average rate of decrease observed in bed rest studies (Ried-Larsen, Aarts, & Joyner, 2017). This rate of decrease is linear over bed rest durations from ∼4 h to 90 days (Ried-Larsen et al., 2017). If we assume, as a first approximation, that the rate of decrease of is linear also following a forced inactivity not associated with bed rest (such as the COVID-19 confinement), over a 2-month period the decrease would be a terrifying −30%! Realistically, during an inactivity such as that elicited by the COVID-19 pandemic, the decrease could be slightly less pronounced, considering that in the studies evaluated by Ried-Larsen et al. (2017) the bed rest was strict, and no countermeasures were provided. But, still, the decrease associated with a prolonged period of forced inactivity would likely be substantial.
The studies mentioned above, were exclusively (Krogh-Madsen et al., 2010), or almost exclusively (Ried-Larsen et al., 2017), conducted on young subjects. What could be the situation in the elderly? Inactivity studies in the elderly are very scarce, mainly for ethical reasons. Some insights could be derived from the limited number of bed rest studies carried out in elderly or middle-aged subjects. In the study by Pišot et al. (2016), for example, the percentage decrease in during a 2-wk bed rest was twice greater in 60-yr old subjects (−15%) vs. that observed in young controls. During a 2 wk-rehabilitation period following the bed rest, moreover, young subjects recovered the pre-bed rest baseline, whereas in the elderly the recovery was minor and incomplete (Pišot et al., 2016). Thus, it is reasonable to assume that also during a period of forced inactivity, not associated with bed rest, the decrease would be more pronounced in the elderly with respect to younger counterparts.
A direct dose–response relationship is observed between exercise “volume” (duration x intensity) and cardiorespiratory fitness. According to Joyner and Green (2009) ∼50% of the protective effects of physical activity are accounted for by a reduction of traditional cardiovascular risk factors, such as high blood pressure and blood lipids. Other protective effects presumably relate to decreased low-grade inflammation of visceral fat tissue and to decreased insulin resistance.
During exercise, sheer stress and other hemodynamic stimuli induce positive effects on the peripheral circulation, favouring vasodilation, proliferation of blood vessels and an anti-atherogenic phenotype. Inactivity inevitably goes in the opposite direction. According to Boyle et al. (2013) a reduction of physical activity to <5000 steps/day for only a few days impairs flow-mediated vasodilation. Preliminary data from our group suggest that 10 days of bed rest induces, in healthy young subjects, an impaired microvascular function, as shown by a blunted blood flow increase during passive leg movement of one leg (an index of nitric oxide [NO]-mediated vasodilation [Gifford & Richardson, 2017]) (Zuccarelli et al., 2020), and by a less pronounced reactive microvascular hyperaemia following a transient ischaemia, in association with signs of impaired NO metabolism (Porcelli et al., 2020).
In terms of mitochondrial respiration in skeletal muscle fibres, the studies dealing with the effects of short-term exposures to bed rest are somewhat controversial. Whereas Miotto et al. (2019) and Dirks et al. (2020) described an impaired mitochondrial function following bed rest periods of 3 and 7 days, respectively, other authors (Larsen et al., 2019; Salvadego et al., 2016; Zuccarelli et al., 2020) did not see impairments following 4 and 10 days of bed rest exposure. An impaired mitochondrial respiration was seen after 21 days of bed rest (Salvadego et al., 2018), confirming the impairment of skeletal muscle oxidative function described in that study by other methods (Salvadego et al., 2018). In a broader perspective, it could be concluded that a few days/weeks of inactivity impair the O2 pathway at all levels, from the cardiovascular system to the oxidative function of skeletal muscles.
“Cardiorespiratory fitness”: effects on health and mortality
is classically considered a variable evaluating the maximal performance of the cardiorespiratory system and skeletal muscles in the transport and in the utilisation of O2 for the purpose of oxidative phosphorylation. Besides being one of the main determinants of exercise tolerance, is considered an index of “cardiorespiratory fitness”. As such, (or a “proxy” of , such as or the number of METs, multiples of resting metabolic rate, that can be reached during exercise) is inversely related to mortality. According to Myers et al. (2002), both in normal subjects and in patients with cardiovascular diseases “exercise capacity (number of METs reached during exercise) is a more powerful predictor of mortality than other established risk factors for cardiovascular diseases”. According to the same authors, for every 1 MET drop in cardiorespiratory fitness mortality increases by 12% (Myers et al., 2002). In an hypothetical sedentary 70-yr subject with a of ∼25 ml kg−1 min−1, a forced inactivity of 4 weeks would likely translate into a ∼15% decrease in (see above), corresponding to a decrease of ∼3.75 ml kg−1 min−1, corresponding to ∼1 MET: this, in turn, would translate into a ∼12% increase in mortality! According to Blair, Kohl, Paffenbarger, Clark, and Gibbons (1989), when cardiorespiratory fitness decreases from 10 to 4 METs the death rate increases ∼4.5 times.
A reduced cardiorespiratory fitness negatively affects mortality also independently from its effects on cardiovascular diseases. According to Booth et al. (2017) for at least 35 chronic diseases/conditions, very relevant in terms of their impact on public health, physical activity has a role in the prevention or as a therapy (see also the review by Pedersen & Saltin, 2015) including: ischaemic heart disease, stroke, hypertension, deep vein thrombosis, chronic heart failure, endothelial dysfunction, peripheral artery disease, type 2 diabetes, metabolic syndrome, osteoporosis, osteoarthritis, falls, balance problems, rheumatoid arthritis, chronic pain, non-alcoholic fatty liver disease, colon cancer, diverticulitis, constipation, breast cancer, ovarian cancer, polycistic ovaric syndrome, gestational diabetes, preeclampsia, cognitive dysfunction, anxiety, depression, sarcopenia, and several others.
Is there a “minimum amount” of exercise to recommend?
What is the minimum amount of exercise needed to prevent the impairment of cardiovascular fitness and prevent, or at least attenuate, the negative health consequences of enforced “lockdown”? Whereas the Physical Activity Guidelines for Americans normally recommend 150–300 min per week of moderate-intensity aerobic physical activity, and 2 sessions per week of muscle strength training, the minimum amount of exercise to recommend in an emergency situation, such as home confinement during the present COVID-19 pandemic, is not clear. Very little is known about this topic, and good quality research is badly needed. According to the 2008 version of the U.S. Physical Activity Guidelines “some physical activity is better than none”. According to Slentz et al. (2007) “a prudent approach would be to recommend that all adults aim for 30 min of moderate-intensity activity each day, and then let body mass changes be the surrogate measure for determining if this amount of activity is adequate”. As mentioned above, a threshold of ∼4500–6000 steps/day has been identified as the minimum required to avoid an increased cardio-metabolic risk (Adams et al., 2019). The vagueness of these recommendations, together with the extraordinary burden of physical inactivity put on hundreds of millions of people by the COVID-19 pandemic, stress the need for more research on the topic.
Awareness of energy intake in physical inactivity to maintain energy balance and prevent metabolic alterations: everything will be all right (Italian motto during the COVID-19 epidemics)
The European population is aging with an increasingly higher percentage of people above 60 years. The absence of vaccines to deal with the sudden COVID-19 pandemic leaves home restriction as the only “therapeutic option”. This countermeasure mainly is going to benefit older people as they seem to be the most affected by the virus. However, domestic restriction has a physio-pathological, psychological and metabolic impact on people.
Physical exercise is a critical element to maintain humans in good health. Humans developed and evolved during ages through continuous physical activity and a human body reaches an optimal physical and mental state when physical activity is balanced with energy intake. While Paleolithic hunter-gatherers (as well as humans living nowadays in a Paleolithic state) are reported to walk up to 16 km per day, civilisation limited walking as a necessity (O'Keefe, Vogel, Lavie, & Cordain, 2010). The effects of reduced mobility have been balanced through history by leisure activities (e.g. sports) but are going to be detrimental in these days, when limitations in walking and outdoor activities are mandatory. This might lead to negative changes in mental and physical status associated with physical inactivity. It is required to define and quantify these alterations in order to counteract their negative effects. In order to maintain body composition and efficiency, a precise matching between exercise-associated energy expenditure and energy intake with nutrition is required.
Negative energy balance
Physical inactivity, bed rest and sedentary lifestyle are associated with decreased activity-associated energy expenditure. Nonetheless, energy intake may not be reduced in parallel with expenditure due to inefficient appetite regulation or to maladaptive behaviour (Panahi & Tremblay, 2018). Indeed, experimental works demonstrate a complex scenario. Experimental bed rest in healthy volunteers as well as long term space-flight are suitable models to investigate physiologic and psychological adaptation to confinement and inactivity. Sixty days of strict bed rest (an experimental approach to study the effects of physical inactivity) in lean healthy women did not change gut hormones or fat mass but reduced muscle mass and, surprisingly, the desire to consume food. In another arm of the study, exercise-induced energy expenditure in bed rest did not induce hunger and directly promoted a negative energy balance (Bergouignan et al., 2010).
The combination of low energy intake and physical inactivity, typically observed in bedridden sick patients, may lead to protein-energy malnutrition, skeletal muscle and fat mass loss, increased complications and, possibly, poor clinical outcome (Ritz & Elia, 1999). Poor energy intake is often observed in astronauts during space missions in microgravity. Astronauts may exhibit alterations in body composition and efficiency commonly observed in bedridden patients (Ritz & Elia, 1999; Wade et al., 2002; Wilson & Morley, 2003). In addition to decreased energy intake, physical inactivity is characterised by anabolic resistance, i.e. a decreased ability to utilise dietary amino acids for synthesis of body proteins. Anabolic resistance to dietary amino acids in association with muscle unloading leads to protein catabolism (Biolo et al., 2004; Ferrando, Lane, Stuart, Davis-Street, & Wolfe, 1996; Stein, Leskiw, Schluter, Donaldson, & Larina, 1999; Stevenson, Giresi, Koncarevic, & Kandarian, 2003) and, ultimately, to muscle dysfunction and atrophy (di Prampero & Narici, 2003; Jackman & Kandarian, 2004). Major triggers of anorexia and decreased food intake in bedridden patients, sedentary healthy humans and astronauts are cytokines and systemic inflammation, disruption of circadian rhythms, alteration in gastrointestinal functions and alterations in neuroendocrine mediators (Da Silva et al., 2002; Stein et al., 1999). Evidence indicates that anorexia in astronauts during long-term space flight can lead to 20–30% decrease in food intake as compared to pre- and/or post-flight conditions (Da Silva et al., 2002; Stein et al., 1999; Wade et al., 2002). By this mechanism, the body weight of an astronaut can decrease by about 0.5 kg for each week spent in space (Wade et al., 2002).
Positive energy balance
In contrast to bedridden sick patients and astronauts, sedentary behaviour in healthy humans may not be associated with decreased appetite. In sedentary healthy humans, humoral and psychological mechanisms of appetite regulation may be altered. Appetite and food intake may not be matched by the decrease in energy requirement associated with inactivity. In this condition, mental work or leisure activities carried out while sedentary may increase the appetite and desire to eat, possibly linked to changes in hormones, neuromediators and gluco-metabolic pattern. Thus, the problem of appetite in sedentariness may not only be attributed to a lack of movement, but also to the stimulation provided by replacing activities (Panahi & Tremblay, 2018). When physical exercise is restricted on condition of sedentary behaviour, energy intake largely depends on psychological mechanisms. Regardless of physiological or psychological mechanisms, positive energy balance in physical inactivity greatly influences metabolic regulation, body composition, muscle efficiency and cardiometabolic risk profile. The combination of positive energy balance with inactivity leads to insulin resistance (Blanc et al., 1998; Stuart et al., 1988), fat accumulation preferentially in the visceral compartments (Olsen, Krogh-Madsen, Thomsen, Booth, & Pedersen, 2008), and lean body mass catabolism (Barbe et al., 1999; Blanc, Normand, Pachiaudi, Duvareille, & Gharib, 2000; Ferrando et al., 1996; Gretebeck, Schoeller, Gibson, & Lane, 1995; Krebs, Schneider, Evans, Kuo, & LeBlanc, 1990; Lovejoy et al., 1999; Scheld et al., 2001; Shackelford et al., 2004; Stein et al., 1999). Excess of food intake, inactivity and fat accumulation trigger a low-grade inflammatory response and enhance oxidative stress (Schaffler, Muller-Ladner, Scholmerich, & Buchler, 2006; Van Guilder, Hoetzer, Greiner, Stauffer, & Desouza, 2006). Inflammation and redox stress lower muscle protein synthesis and accelerate proteolysis (Powers, Kavazis, & McClung, 2007; Schaap, Pluijm, Deeg, & Visser, 2006). It was demonstrated that, in animal muscle, overfeeding lowered protein fractional synthesis rate (Glick, McNurlan, & Garlick, 1982). While, in conditions of activated systemic inflammation and redox imbalance, the rate of utilisation of the tripeptide glutathione, the major cellular defender against oxidative stress, is accelerated (Lu, 1999; Richards, Roberts, Dunstan, McGregor, & Butt, 1998).
Another important component to take in account is ghrelin. This is a circulating hormone produced by enteroendocrine cells especially in the stomach. It is often called a “hunger hormone” because it increases food intake. Blood levels of ghrelin are highest before meals and return to lower levels after feeding. Ghrelin response is altered during overfeeding and may contribute to muscle catabolism (Nagaya et al., 2005; Robertson, Henderson, Vist, & Rumsey, 1998).
We tested the hypothesis that during inactivity (bed rest), positive energy balance leading to fat deposition would accelerate inactivity-induced loss of lean mass and activation of systemic inflammation, free radical production and antioxidant defenses (Biolo et al., 2007). We demonstrated that, during 35 days of bed rest in healthy young volunteers at different levels of energy intake, fat gain was associated with the greatest loss of skeletal muscle mass. Moreover, we also found that a positive energy balance during experimental inactivity, greatly activated the glutathione system (Lu, 1999), providing both local and systemic antioxidant protection (Richards et al., 1998). In contrast, maintenance of near-neutral balance (no significant change in body fat) during bed rest was associated with lower muscle loss and no alteration in systemic inflammation, redox balance and glutathione synthesis. Evidence indicates that proinflammatory mediators up-regulates glutathione synthesis and oxidative stress (Lu, 1999). Plasma C-reactive protein and myeloperoxidase are suitable markers for detecting activation of systemic inflammation (Podrez, Abu-Soud, & Hazen, 2000). After 5 weeks of bed rest at positive energy balance, C-reactive protein levels were higher (p = .04) than in subjects with neutral balance (Biolo et al., 2007). The effects of inactivity and overfeeding on systemic inflammation and redox balance can contribute to muscle mass catabolism during bed rest at positive energy balance (Glick et al., 1982; Powers et al., 2007; Schaap et al., 2006).
We also investigated changes of TNF related apoptosis induction ligand (TRAIL) following bed rest at different levels of energy intake. We showed a strict relationship between TRAIL and levels of energy intake during sedentariness. TRAIL was significantly higher in overfed subjects as compared to those following an eucaloric diet. Energy restriction significantly decreased circulating TRAIL. (Biolo, Secchiero, De Giorgi, Tisato, & Zauli, 2012).
Long-term physical inactivity affected also lipid metabolism (Mazzucco, Agostini, Mangogna, Cattin, & Biolo, 2010). Inactivity, in fact, led to insulin resistance and dyslipidemia, namely an increased levels of triglycerides associated with decreased HDL concentration. CETP is a plasma protein transferring cholesteryl esters and triglycerides from HDL to VLDL and LDL. We have demonstrated that its availability significantly increased after bed rest (Mazzucco et al., 201) explaining how inactivity decreased the ratio between HDL and non-HDL cholesterol. We suggest, therefore, that changes in CETP availability contributes to inactivity-mediated alterations of plasma lipid pattern.
In media stat virtus
Physical inactivity is frequently associated with spontaneous reduction in caloric intake especially in stress conditions such as acute or chronic diseases or long-term space flight. Loss of muscle mass in persons with very low physical activity is faster when energy intake is not adequate and this alteration may rapidly lead to severe malnutrition. This catabolic response may be further amplified by stress mediators, such as cortisol and cytokines. Other potential causes for this weight loss may involve variations in circadian rhythms and busy work schedules.
In contrast to sick or stressed people, reduction of physical activity in healthy humans may lead to excess nutrient intake. It has been shown that, excess fat deposition during physical inactivity is associated with greater muscle loss and greater activation of systemic inflammation and antioxidant defenses. These mechanisms potentially contribute to long-term changes in body composition and to development of cardiometabolic risk in healthy sedentary persons.
Media and science communicators often represent energy balance as the mathematical difference between energy expenditure and energy intake. Nonetheless, food intake and energy expenditure are not independent variables and may influence each other to complicate the physiological scenario and therapeutic strategies. Psychology and personal behaviour further complicate such relationship between food intake and energy expenditure. Increasing the awareness of physiological and psychological mechanisms of overfeeding will contribute to the maintenance of energy balance and metabolic health in conditions of reduced physical activity.
Physical inactivity during COVID-19: nutritional strategies to counteract its effects on metabolism and body composition
The perfect storm
Humans’ evolutionary history suggests that our ancestors were forced to be physically active in order to survive (hunters-gatherers). Only in the last few centuries physical activity has became a leisure/hobby and, until recently, only for the rich and noble. In fact, the treadmill was invented in England 200 years ago as a prison rehabilitation device (Shayt, 1989) but was banned as a cruel and inhumane practice at the beginning of the 1900s (BMJ, 1885). Hunters-gatherers were forced to walk and run during daily activity and also, during non-ambulatory rest, they performed many movements that increase muscle activity unlike the typical sedentary posture of industrialised populations (Raichlen et al., 2020). This fact may explain, in part, the paradoxical negative effect of physical inactivity (PI) on health, considering the evolutionary pressure to save energy. The other side of the coin is, obviously, diet. Even though the diet-centric paradigm has been demonstrated to be partially, flawed (Archer, Lavie, & Hill, 2018), energy intake, dietary nutrients composition, and distribution influence health outcomes and body fat. In this regard it has been demonstrated that physical activity (PA) is important not only for its effects on energy expenditure but also for its influence on energy intake (Shook et al., 2015; Stubbs et al., 2004). That being said, it follows that the relationship between PA and metabolic control is more complex that a simple increase or decrease of energy expenditure; PA and its influence on metabolic flux (liver and muscle glycogen, adipose tissue liposynthesis and lipolysis) may be considered, quite rightly, the major determinant of energy control (energy intake and energy expenditure) and of metabolic control. It follows that PI and sedentary behaviour have a clear negative effect on health. The two terms “physical inactivity” and “sedentary behaviour” have been recently defined (Tremblay et al., 2017) as “an insufficient physical activity level to meet present physical activity recommendations (i.e. for adults (≥ 18 years): not achieving 150 min of moderate-to-vigorous-intensity physical activity per week or 75 min of vigorous-intensity physical activity per week or an equivalent combination of moderate- and vigorous-intensity activity)” and “any waking behaviour characterized by an energy expenditure ≤1.5 metabolic equivalents (METs), while in a sitting, reclining or lying posture”, respectively. It is clear that the recent, COVID-19-related strict limitation to mobility in many countries and the prohibition of moving from home unless for reasons related to work, real necessity or health care, have drastically reduced the citizens’ possibility to walk, run and to exercise in gyms, swimming pools, etc. We define this situation as being more related to PI than to sedentary behaviour, even though the forced lockdown may exacerbate previous bad sedentary habits (i.e. increasing the time spent lying, sitting, etc). Another dangerous factor is the increase of the number of hours devoted to television watching: high levels of moderate intensity PA (60–75 min per day) eliminates the increased risk of death associated with great sitting time but only blunts the increased risk associated with high TV-viewing time (Ekelund et al., 2016). During this period of home isolation, a good indicator of PI is the step-reduction. Many studies have investigated the effects of step-reduction on health parameters, demonstrating that even a short-term reduction in PA has a negative effect on skeletal muscle protein and carbohydrate metabolism. These changes may lead to muscle anabolic resistance, muscle and adipose tissue insulin resistance, and liver triglyceride accumulation with consequent hepatic insulin resistance. The final result is dyslipidaemia, a decrease of muscle mass and strength and, in general, an overall decline in function. Thus, the obligation to stay at home, the high number of tv “on-demand” channels, the increase in spare time, boredom and hunger represent the “perfect storm” for a dramatic future increase of metabolic diseases.
Exercise and nutritional countermeasures to physical inactivity and its consequences
Obviously, the best countermeasure to PI is PA, i.e. trying to exercise even when confined at home; but it is also of paramount importance to modulate the diet to fit the new physical activity context.
In general, many studies provide strong bases for amino acids/protein supplementation in older adults (Volpi et al., 2013) whilst the existence of anabolic resistance related to age is not well defined (Moro et al., 2018). Anyhow, in older healthy adults and healthy adults the ability of amino acids/protein supplementation to improve muscle mass/function is related to the amount and the kind of exercise performed (Churchward-Venne, Holwerda, Phillips, & van Loon, 2016; Morton et al., 2018; Morton, McGlory, & Phillips, 2015). Resistance training, that can be done without the so-called free weights (barbells, dumbbells, kettlebells) but also with bodyweight exercises (Suchomel, Nimphius, Bellon, & Stone, 2018), is the best choice to maintain or increase muscle mass and function. Subjects requested to stay at home during this time of social distancing and isolation should modify their diet according to the reduced activity-induced energy expenditure (up to 35–40%) (EVIDATION, 2020), reducing the total energy intake by about 15–20% (the average activity-induced energy expenditure in general population is about one-third of total energy expenditure) (Westerterp, 2003). It is important to refrain from multiple snacks during the day (nibbling) because, if not well controlled, this behaviour risks an increase in daily energy intake. In addition, in this period, social distancing, isolation and concerns about COVID-19 may increase depression, anxiety and boredom (Wang et al., 2020), factors which are related to an increase of energy intake (Braden, Musher-Eizenman, Watford, & Emley, 2018); thus, it would be helpful to maintain 2–3 meals per day, with a long overnight fast. Kahleova and colleagues (Kahleova, Lloren J, Mashchak, Hill, & Fraser G, 2017) investigated more than 50 thousand adult members of Seventh-day Adventist churches in the United States and Canada. The results showed that eating 1 or 2 meals daily was associated with better health outcomes compared with 3 meals daily. The Seventh-day Adventist is a unique population in which the consumption of alcohol, tobacco, and pork is prohibited and the majority of members adhere to a lacto-ovovegetarian diet (Beeson, Mills, Phillips, Andress, & Fraser, 1989; Phillips, Lemon, Beeson, & Kuzma, 1978). This religious group has a low meal frequency and also a regular meal timing that, together, may positively influence their health (Paoli, Tinsley, Bianco, & Moro, 2019). Seventh-day Adventists have an early dinner and a prolonged fast until breakfast. The long period of fasting may have beneficial effects on inflammation (Paoli et al., 2019; Vasconcelos et al., 2014) and immune system response (Faris et al., 2012; Han et al., 2018; Mindikoglu et al., 2020). We demonstrated that in healthy subjects (Moro et al., 2016) a normal energy time-restricted eating protocol (i.e. a window of 16 h of fasting and a window of 8 h of eating) may reduce many markers of inflammation such as tumour necrosis factor alpha, interleukin 6, and interleukin 1 beta and, at the same time, may increase the anti-inflammatory cytokine adiponectin. Also the energy distribution during the day is important: Jakubowicz, Barnea, Wainstein, and Froy (2013) demonstrated that diets with the same energy but differing in the distribution of calories during the day (high calorie in the morning vs. high calorie in the evening) may have influences on body weight, insulin resistance indices, and subjective appetite feeling in overweight/obese women. These suggest that is preferable for health to consume more calories earlier in the day (breakfast).
We therefore posit that during “stay at home” period, the following dietary practices may be beneficial:•a reduced meal frequency, regular meals and a long fasting period between dinner and breakfast (i.e. more than 12 h);•a reduced energy intake (from 15 up to 20–25%) compared to usual;•consumption of fresh vegetables (if possible), good quality protein sources (fish, poultry, lean meat);•at least 1.3 grams of good quality protein per kilogram of body weight (for an average subjects of 70 Kg it means 91 grams of protein, divided equally between meals);•moderate consumptions of seed and nuts and monounsaturated fat e.g. olive oil, due to the high energy content of fats;•avoid refined foods;•reduce the intake of high glycaemic index, glycaemic load and/or high insulinemic foods;•consume more energy during breakfast (about 40%), less during lunch (30%) and dinner (30%).
In these strange times that reflect some life habits of the mediaeval period, it may be useful to follow this twelfth-century recommendation: “Eat like a king in the morning, a prince at noon, and a peasant at dinner”
Take-home messages
Neuromuscular system
•
Sedentarism causes a very rapid loss of muscle mass, detectable after just two days from the onset of inactivity; after 10 days the loss of muscle mass is ∼ 6% and after 30 days ∼10%
•
Inactivity also leads to degenerative changes of the neuromuscular system: signs of damage to the neuromuscular junction are found after just 10 days and signs of denervation can be observed after just 3-days of inactivity
•
Daily exercise is essential for counteracting the effects of inactivity: low to medium-intensity, high volume resistive exercise seems ideal for preventing neuromuscular degeneration, maximising protein synthesis and combating muscle atrophy
•
Neuromuscular integrity is closely linked to mitochondrial function, hence a combination of aerobic as well as low-intensity, high-volume strength training are likely to afford protection against neurodegenerative changes and muscle atrophy
Muscle protein metabolism
•
Physical inactivity and time spent sitting increase risk of poor metabolic health, functional decline and all-cause mortality
•
Suppression of muscle protein synthesis is the primary driver of muscle mass loss during immobilisation or step count reduction in young, healthy people, and is evident within days
•
The precise cellular and molecular mechanisms responsible for the decline in muscle mass observed during immobilisation in humans remain to be elucidated
•
We do not yet fully understand the interaction between ageing processes and inactivity induced muscle mass loss
•
The precise relationship between exercise dose (daily frequency and intensity) and muscle mass retention during prolonged periods of immobilisation or inactivity is not yet clear, but muscle contraction is a very effective countermeasure to dampen muscle mass loss during inactivity in young volunteers, although maybe less so in older people
•
It will take several months to restore muscle mass loss completely following prolonged periods of inactivity or immobilisation in the absence of structured rehabilitation exercise
Glucose homeostasis
•
Skeletal muscle has a pivotal role in inactivity-induced insulin resistance
•
Inactivity leads to a specific reduction in muscle insulin sensitivity without affecting that of the liver
•
Just few days of step-reduction can induce insulin resistance
•
Changes in insulin sensitivity precede muscle atrophy and changes in body composition
•
Start monitoring your physical activity (smart-phone, wearables)
•
Strive to achieve >5000 steps per day
•
Any form of energy expenditure is of help to avoid the deleterious effects of sedentarism;
•
If possible, go outside in the nature (walking, jogging, running)
•
The advices are important for all, but particularly important for people at risk of diabetes (family history of diabetes) and cardio-vascular disease (elevated blood pressure, overweight/obese, elevated cholesterol, smokers)
Cardiorespiratory system
•
A reduced level of physical activity is inevitably associated with a reduced “cardiorespiratory fitness”, as estimated by the maximal O2 uptake (VO2max) or by other variables
•
Various steps along the O2 pathway are impaired by inactivity, from central and peripheral cardiovascular function to skeletal muscle oxidative metabolism
•
During profound inactivity the rate of loss of VO2max (about −0.5%/day) is similar to that described in bed rest studies. An accelerated decrease may occur in middle-aged and elderly subjects
•
A lower or decreased VO2max is associated with an increased mortality
•
The minimum amount of aerobic exercise needed to counteract the VO2max decrease due to inactivity is not clear. More research is needed. A reasonable estimate could be 4500–6000 steps/day
Energy balance, inflammation, lean and fat body mass
•
Overfeeding and excess fat deposition in healthy sedentary persons is associated with greater muscle loss and activation of systemic inflammation, leading to development of cardio-metabolic risk
•
Increasing the awareness of physiological and psychological mechanisms of overfeeding will contribute to the maintenance of energy balance and metabolic health of sedentary persons
•
Bed rest or inactivity in patients with diseases or in subjects in stressed conditions (e.g. strict home confinements or extreme environments) may be associated with decreased energy intake, rapidly leading to muscle wasting. Nutritional support and/or anabolic countermeasures may be required
Nutritional intake, metabolism and body composition
•
Subjects requested to stay at home during this time of social distancing and isolation reduce their daily activity-induced energy expenditure up to 35–40%;
•
The obligation to stay at home, the high number of tv “on-demand” channels, the increase of spare time, boredom and hunger represent the “perfect storm” for a dramatic future increase of metabolic diseases;
Practical suggestions
•
Reduce the daily energy intake (from 15 up to 20–25%) compared to usual;
•
Consume more fresh vegetables (if possible), good quality protein sources (fish, poultry, lean meat);
•
Consume at least 1.3 grams of good quality protein per kilogram of body weight.
•
Consume (moderately due to the high energy content) seeds. nuts and monounsaturated fats e.g. olive oil;
•
Avoid refined foods
•
Reduce the intake of high glycaemic index, glycaemic load and/or high insulinemic foods;
•
A reduced meal frequency, regular meals and a long fasting period between dinner and breakfast (i.e. more than 12 hours) may have some beneficial effects on metabolism and some health outcomes
•
Consume more energy during breakfast (about 40% of daily total), less during lunch (30% of daily total) and dinner (30% of daily total)
Disclosure statement
No potential conflict of interest was reported by the author(s).
Funding
This work was funded by ASI, MARS-PRE Project, n. DC-VUM-2017-006.
References
Aagaard, P., Magnusson, P. S., Larsson, B., Kjaer, M., & Krustrup, P. (2007). Mechanical muscle function, morphology, and fiber type in lifelong trained elderly. Medicine & Science in Sports & Exercise, 39(11), 1989–1996. Crossref. PubMed.
Abadi, A., Glover, E. I., Isfort, R. J., Raha, S., Safdar, A., Yasuda, N., … Tarnopolsky, M. (2009). Limb immobilization induces a coordinate down-regulation of mitochondrial and other metabolic pathways in men and women. PLoS One, 4(8), e6518. Crossref. PubMed.
Adams, B., Fidler, K., Demoes, N., Aguiar, E. J., Ducharme, S. W., McCullough, A. K., … Thomas, D. (2019). Cardiometabolic thresholds for peak 30-min cadence and steps/day. PLoS One, 14(8), e0219933. Crossref. PubMed.
Alibegovic, A. C., Hojbjerre, L., Sonne, M. P., Van, H. G., Stallknecht, B., Dela, F., & Vaag, A. (2009). Impact of 9 days of bed rest on hepatic and peripheral insulin action, insulin secretion, and whole-body lipolysis in healthy young male offspring of patients with type 2 diabetes. Diabetes, 58, 2749–2756. Crossref. PubMed.
Alibegovic, A. C., Sonne, M. P., Hojbjerre, L., Bork-Jensen, J., Jacobsen, S., Nilsson, E., … Vaag, A. (2010). Insulin resistance induced by physical inactivity is associated with multiple transcriptional changes in skeletal muscle in young men. American Journal of Physiology-Endocrinology and Metabolism, 299, E752–E763. Crossref. PubMed.
Alkner, B. A., & Tesch, P. A. (2004a). Efficacy of a gravity-independent resistance exercise device as a countermeasure to muscle atrophy during 29-day bed rest. Acta Physiologica Scandinavica, 181(3), 345–357.Crossref. PubMed.
Alkner, B. A., & Tesch, P. A. (2004b). Knee extensor and plantar flexor muscle size and function following 90 days of bed rest with or without resistance exercise. European Journal of Applied Physiology, 93(3), 294–305. Crossref. PubMed.
Archer, E., Lavie, C. J., & Hill, J. O. (2018). The contributions of ‘diet’, ‘genes’, and physical activity to the etiology of obesity: Contrary evidence and consilience. Progress in Cardiovascular Diseases, 61(2), 89–102. Crossref. PubMed.
Arciero, P. J., Smith, D. L., & Calles-Escandon, J. (1998). Effects of short-term inactivity on glucose tolerance, energy expenditure, and blood flow in trained subjects. Journal of Applied Physiology, 84, 1365–1373. Crossref. PubMed.
Arentson-Lantz, E. J., English, K. L., Paddon-Jones, D., & Fry, C. S. (2016). Fourteen days of bed rest induces a decline in satellite cell content and robust atrophy of skeletal muscle fibers in middle-aged adults. Journal of Applied Physiology, 120(8), 965–975. Crossref. PubMed.
Atherton, P. J., Babraj, J., Smith, K., Singh, J., Rennie, M. J., & Wackerhage, H. (2005). Selective activation of AMPK-PGC-1alpha or PKB-TSC2-mTOR signaling can explain specific adaptive responses to endurance or resistance training-like electrical muscle stimulation. The FASEB Journal, 19, 786–788. Crossref. PubMed.
Barbe, P., Galitzky, J., Thalamas, C., Langin, D., Lafontan, M., Senard, J. M., & Berlan, M. (1999). Increase in epinephrine-induced responsiveness during microgravity simulated by head-down bed rest in humans. Journal of Applied Physiology, 87(5), 1614–1620. Crossref. PubMed.
Beeson, W. L., Mills, P. K., Phillips, R. L., Andress, M., & Fraser, G. E. (1989). Chronic disease among seventh-day adventists, a low-risk group. Rationale, methodology, and description of the population. Cancer, 64(3), 570–581.Crossref. PubMed.
Belavý, D. L., Miokovic, T., Armbrecht, G., Rittweger, J., & Felsenberg, D. (2009). Resistive vibration exercise reduces lower limb muscle atrophy during 56-day bed-rest. Journal of Musculoskeletal & Neuronal Interactions, 9(4), 225–235. PubMed.
Benatti, F. B., Larsen, S. A., Kofoed, K., Nielsen, S. T., Harder-Lauridsen, N. M., Lyngbaek, M. P., … Ried-Larsen, M. (2017). Intermittent standing but not a moderate exercise bout reduces postprandial glycemia. Medicine & Science in Sports & Exercise, 49, 2305–2314. Crossref. PubMed.
Bergouignan, A., Momken, I., Schoeller, D. A., Normand, S., Zahariev, A., Lescure, B., … Blanc, S. (2010). Regulation of energy balance during long-term physical inactivity induced by bed rest with and without exercise training. The Journal of Clinical Endocrinology & Metabolism, 95(3), 1045–1053. Crossref. PubMed.
Bienso, R. S., Ringholm, S., Kiilerich, K., Aachmann-Andersen, N. J., Krogh-Madsen, R., Guerra, B., … Wojtaszewski, J. F. (2012). GLUT4 and glycogen synthase are key players in bed rest-induced insulin resistance. Diabetes, 61, 1090–1099. Crossref. PubMed.
Biolo, G., Agostini, F., Simunic, B., Sturma, M., Torelli, L., Preiser, J. C., … Narici, M. V. (2008). Positive energy balance is associated with accelerated muscle atrophy and increased erythrocyte glutathione turnover during 5 wk of bed rest. The American Journal of Clinical Nutrition, 88(4), 950–958. Crossref. PubMed.
Biolo, G., Ciocchi, B., Lebenstedt, M., Barazzoni, R., Zanetti, M., Platen, P., … Guarnieri, G. (2004). Short-term bed rest impairs amino acid-induced protein anabolism in humans. The Journal of Physiology, 558(2), 381–388.Crossref. PubMed.
Biolo, G., Secchiero, P., De Giorgi, S., Tisato, V., & Zauli, G. (2012). The energy balance positively regulates the levels of circulating TNF-related apoptosis inducing ligand in humans. Clinical Nutrition, 31(6), 1018–1021.Crossref. PubMed.
Blackwell, J., Atherton, P. J., Smith, K., Doleman, B., Williams, J. P., Lund, J. N., & Phillips, B. E. (2017). The efficacy of unsupervised home-based exercise regimens in comparison to supervised laboratory-based exercise training upon cardio-respiratory health facets. Physiological Reports, 5(17), e13390. Crossref. PubMed.
Blair, S. N. (2009). Physical inactivity: The biggest public health problem of the 21st century. British Journal of Sports Medicine, 43, 1–2. Crossref. PubMed.
Blair, S. N., Kohl, H. W., Paffenbarger, R. S., Clark, D. G., & Gibbons, L. W. (1989). Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA, 262, 2395–2401. Crossref. PubMed.
Blanc, S., Normand, S., Pachiaudi, C., Duvareille, M., & Gharib, C. (2000). Leptin responses to physical inactivity induced by simulated weightlessness. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 279, R891–R898. Crossref. PubMed.
Blanc, S., Normand, S., Ritz, P., Pachiaudi, C., Vico, L., Gharib, C., & Gauquelin-Koch, G. (1998). Energy and water metabolism, body composition, and hormonal changes induced by 42 days of enforced inactivity and simulated weightlessness. Journal of Clinical Endocrinology and Metabolism, 83(12), 4289–4297. PubMed.
Blotner, H. (1945). Effect of prolonged physical inactivity on tolerance of sugar. Archives of Internal Medicine, 75, 39–44. Crossref.
Bodine, S. C., Stitt, T. N., Gonzalez, M., Kline, W. O., Stover, G. L., Bauerlein, R., … Yancopoulos, G. D. (2001). Akt/mTOR pathway is a crucial regulator of skeletal muscle hypertrophy and can prevent muscle atrophy in vivo. Nature Cell Biology, 3(11), 1014–1019. Crossref. PubMed.
Booth, F. W., Roberts, C. K., Thyfault, J. P., Rugsegger, G. N., & Toedebusch, R. G. (2017). Role of inactivity in chronic diseases: Evolutionary insight and pathophysiological mechanisms. Physiological Reviews, 97, 1351–1402. Crossref. PubMed.
Boyle, L. J., Credeur, D. P., Jenkins, N. T., Padilla, J., Leidy, H. J., Thyfault, J. P., & Fadel, P. J. (2013). Impact of reduced daily physical activity on conduit artery flow-mediated dilation and circulating endothelial microparticles. Journal of Applied Physiology, 115, 1519–1525. Crossref. PubMed.
Braden, A., Musher-Eizenman, D., Watford, T., & Emley, E. (2018). Eating when depressed, anxious, bored, or happy: Are emotional eating types associated with unique psychological and physical health correlates? Appetite, 125, 410–417. Crossref. PubMed.
Breen, L., Stokes, K. A., Churchward-Venne, T. A., Moore, D. R., Baker, S. K., Smith, K., … Phillips, S. M. (2013). Two weeks of reduced activity decreases leg lean mass and induces “anabolic resistance” of myofibrillar protein synthesis in healthy elderly. The Journal of Clinical Endocrinology & Metabolism, 98(6), 2604–2612. Crossref. PubMed.
British Medical Journal. (1885). Death on the treadmill. BMJ, 1(1265), 667–668.
Burd, N. A., West, D. W., Staples, A. W., Atherton, P. J., Baker, J. M., Moore, D. R., … Phillips, S. M. (2010). Low-load high volume resistance exercise stimulates muscle protein synthesis more than high-load low volume resistance exercise in young men. PLoS One, 5(8), e12033. Crossref. PubMed.
Churchward-Venne, T. A., Holwerda, A. M., Phillips, S. M., & van Loon, L. J. (2016). What is the optimal amount of protein to support post-exercise skeletal muscle reconditioning in the older adult? Sports Medicine, 46(9), 1205–1212. Crossref. PubMed.
Crossland, H., Skirrow, S., Puthucheary, Z. A., Constantin-Teodosiu, D., & Greenhaff, P. L. (2019). The impact of immobilisation and inflammation on the regulation of muscle mass and insulin resistance: Different routes to similar end-points. The Journal of Physiology, 597, 1259–1270. Crossref. PubMed.
Cuthbertson, D. P. (1929). The influence of prolonged muscular rest on metabolism. Biochemical Journal, 23(6), 1328–1345. Crossref. PubMed.
Da Silva, M. S., Zimmerman, P. M., Meguid, M. M., Nandi, J., Ohinata, K., Xu, Y., … Inui, A. (2002). Anorexia in space and possible etiologies: An overview. Nutrition, 18(10), 805–813. Crossref. PubMed.
de Boer, M. D., Maganaris, C. N., Seynnes, O. R., Rennie, M. J., & Narici, M. V. (2007). Time course of muscular, neural and tendinous adaptations to 23 day unilateral lower-limb suspension in young men. The Journal of Physiology, 583(3), 1079–1091. Crossref. PubMed.
de Boer, M. D., Selby, A., Atherton, P., Smith, K., Seynnes, O. R., Maganaris, C. N., … Rennie, M. J. (2007). The temporal responses of protein synthesis, gene expression and cell signalling in human quadriceps muscle and patellar tendon to disuse. The Journal of Physiology, 585, 241–251. Crossref. PubMed.
Demangel, R., Treffel, L., Py, G., Brioche, T., Pagano, A. F., Bareille, M. P., … Millet, C. (2017). Early structural and functional signature of 3-day human skeletal muscle disuse using the dry immersion model. The Journal of Physiology, 595(13), 4301–4315. Crossref. PubMed.
de Rezende, L. F., Rey-López, J. P., Matsudo, V. K., & do Carmo Luiz, O. (2014). Sedentary behaviour and health outcomes among older adults: A systematic review. BMC Public Health, 14, 333. Crossref. PubMed.
Dickson, G., Gower, H. J., Barton, C. H., Prentice, H. M., Elsom, V. L., Moore, S. E., … Walsh, F. S. (1987). Human muscle neural cell adhesion molecule (N-CAM): Identification of a muscle-specific sequence in the extracellular domain. Cell, 50(7), 1119–1130. Crossref. PubMed.
di Prampero, P. E., & Narici, M. V. (2003). Muscles in microgravity: From fibres to human motion. Journal of Biomechanics, 36, 403–412. Crossref. PubMed.
Dirks, M. L., Miotto, P. M., Goossens, G. H., Senden, J. M., Petrick, H. L., van Kranenburg, J., … Holloway, G. P. (2020). Short-term bed rest-induced insulin resistance cannot be explained by increased mitochondrial H2O2emission. The Journal of Physiology, 598, 123–137. Crossref. PubMed.
Dolkas, C. B., & Greenleaf, J. E. (1977). Insulin and glucose responses during bed rest with isotonic and isometric exercise. Journal of Applied Physiology, 43, 1033–1038. Crossref. PubMed.
Dunstan, D. W., Kingwell, B. A., Larsen, R., Healy, G. N., Cerin, E., Hamilton, M. T., … Owen, N. (2012). Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care, 35(5), 976–983.Crossref. PubMed.
Dunstan, D. W., Salmon, J., Owen, N., Armstrong, T., Zimmet, P. Z., Welborn, T. A., … Shaw, J. E. (2005). Associations of TV viewing and physical activity with the metabolic syndrome in Australian adults. Diabetologia, 48, 2254–2261. Crossref. PubMed.
Duvivier, B. M., Schaper, N. C., Bremers, M. A., Van, C. G., Menheere, P. P., Kars, M., & Savelberg, H. H. (2013). Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLoS One, 8, e55542. Crossref. PubMed.
Duvivier, B. M., Schaper, N. C., Hesselink, M. K., Van, K. L., Stienen, N., Winkens, B., … Savelberg, H. H. (2017). Breaking sitting with light activities vs structured exercise: A randomised crossover study demonstrating benefits for glycaemic control and insulin sensitivity in type 2 diabetes. Diabetologia, 60, 490–498. Crossref. PubMed.
Ekelund, U., Steene-Johannessen, J., Brown, W. J., Fagerland, M. W., Owen, N., Powell, K. E., & Bauman, A. (2016). Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. The Lancet, 388(10051), 1302–1310. Crossref. PubMed.
Ekelund, U., Tarp, J., Steene-Johannessen, J., Hansen, B. H., Jefferis, B., Fagerland, M. W., … Lee, I. M. (2019). Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonised meta-analysis. BMJ, 366, l4570. Crossref. PubMed.
Eriksen, L., Dahl-Petersen, I., Haugaard, S. B., & Dela, F. (2007). Comparison of the effect of multiple short-duration with single long-duration exercise sessions on glucose homeostasis in type 2 diabetes mellitus. Diabetologia, 50, 2245–2253. Crossref. PubMed.
EVIDATION. (2020, March 27). COVID-19 pulse: Delivering weekly insights on the pandemic from a 150,000+ person connected cohort. Retrieved from https://evidation.com/news/covid-19-pulse-first-data-evidation/
Faris, M. A., Kacimi, S., Al-Kurd, R. A., Fararjeh, M. A., Bustanji, Y. K., Mohammad, M. K., & Salem, M. L. (2012). Intermittent fasting during Ramadan attenuates proinflammatory cytokines and immune cells in healthy subjects. Nutrition Research, 32(12), 947–955. Crossref. PubMed.
Ferrando, A. A., Lane, H. W., Stuart, C. A., Davis-Street, J., & Wolfe, R. R. (1996). Prolonged bed rest decreases skeletal muscle and whole body protein synthesis. American Journal of Physiology, 270, E627–E633. PubMed.
Fisher, S. R., Goodwin, J. S., Protas, E. J., Kuo, Y. F., Graham, J. E., Ottenbacher, K. J., & Ostir, G. V. (2011). Ambulatory activity of older adults hospitalized with acute medical illness. Journal of the American Geriatrics Society, 59(1), 91–95. Crossref. PubMed.
Ford, E. S., Schulze, M. B., Kröger, J., Pischon, T., Bergmann, M. M., & Boeing, H. (2010). Television watching and incident diabetes: Findings from the European prospective investigation into cancer and nutrition-Potsdam study. Journal of Diabetes, 2(1), 23–27. Crossref. PubMed.
Friedrichsen, M., Ribel-Madsen, R., Mortensen, B., Hansen, C. N., Alibegovic, A. C., Hojbjerre, L., … Vaag, A. (2012). Muscle inflammatory signaling in response to 9 days of physical inactivity in young men with low compared to normal birth weight. European Journal of Endocrinology, 167, 828–838. Crossref.
Gibbs, B. B., Kowalsky, R. J., Perdomo, S. J., Grier, M., & Jakicic, J. M. (2017). Energy expenditure of deskwork when sitting, standing or alternating positions. Occupational Medicine, 67, 121–127. Crossref. PubMed.
Gifford, J. R., & Richardson, R. S. (2017). CORP: Ultrasound assessment of vascular function with the passive leg movement technique. Journal of Applied Physiology, 123, 1708–1720. Crossref. PubMed.
Glick, Z., McNurlan, M. A., & Garlick, P. J. (1982). Protein synthesis rate in liver and muscle of rats following four days of overfeeding. The Journal of Nutrition, 112, 391–397. Crossref. PubMed.
Glover, E. I., Phillips, S. M., Oates, B. R., Tang, J. E., Tarnopolsky, M. A., Selby, A., … Rennie, M. J. (2008). Immobilization induces anabolic resistance in human myofibrillar protein synthesis with low and high dose amino acid infusion. The Journal of Physiology, 586(24), 6049–6061. Crossref. PubMed.
Grassi, B., Cerretelli, P., Narici, M. V., & Marconi, C. (1991). Peak anaerobic power in master athletes. European Journal of Applied Physiology and Occupational Physiology, 62(6), 394–399. Crossref. PubMed.
Gretebeck, R. J., Schoeller, D. A., Gibson, E. K., & Lane, H. W. (1995). Energy expenditure during antiorthostatic bed rest (simulated microgravity). Journal of Applied Physiology, 78, 2207–2211. Crossref. PubMed.
Hamburg, N. M., McMackin, C. J., Huang, A. L., Shenouda, S. M., Widlansky, M. E., Schulz, E., … Vita, J. A. (2007). Physical inactivity rapidly induces insulin resistance and microvascular dysfunction in healthy volunteers. Arteriosclerosis, Thrombosis, and Vascular Biology, 27, 2650–2656. Crossref. PubMed.
Han, K., Nguyen, A., Traba, J., Yao, X., Kaler, M., Huffstutler, R. D., … Sack, M. N. (2018). A pilot study to investigate the immune-modulatory effects of fasting in steroid-naive mild asthmatics. The Journal of Immunology, 201(5), 1382–1388. Crossref. PubMed.
Healy, G. N., Dunstan, D. W., Salmon, J., Cerin, E., Shaw, J. E., Zimmet, P. Z., & Owen, N. (2008). Breaks in sedentary time: Beneficial associations with metabolic risk. Diabetes Care, 31(4), 661–666. Crossref. PubMed.
Hettwer, S., Dahinden, P., Kucsera, S., Farina, C., Ahmed, S., Fariello, R., … Vrijbloed, J. W. (2013). Elevated levels of a C-terminal agrin fragment identifies a new subset of sarcopenia patients. Experimental Gerontology, 48(1), 69–75. Crossref. PubMed.
Hirsch, C. H., Sommers, L., Olsen, A., Mullen, L., & Winograd, C. H. (1990). The natural history of functional morbidity in hospitalized older patients. Journal of the American Geriatrics Society, 38(12), 1296–1303.Crossref. PubMed.
Hu, F. B., Li, T. Y., Colditz, G. A., Willett, W. C., & Manson, J. E. (2003). Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA, 289(14), 1785–1791.Crossref. PubMed.
Jackman, R. W., & Kandarian, S. C. (2004). The molecular basis of skeletal muscle atrophy. American Journal of Physiology-Cell Physiology, 287, C834–C843. Crossref. PubMed.
Jakubowicz, D., Barnea, M., Wainstein, J., & Froy, O. (2013). High caloric intake at breakfast vs. dinner differentially influences weight loss of overweight and obese women. Obesity, 21(12), 2504–2512. Crossref. PubMed.
Joyner, M. J., & Green, D. J. (2009). Exercise protects the cardiovascular system: Effects beyond traditional risk factors. The Journal of Physiology, 587, 5551–5558. Crossref. PubMed.
Kahleova, H., Lloren J, I., Mashchak, A., Hill, M., & Fraser G, E. (2017). Meal frequency and timing are associated with changes in body mass index in adventist health study 2. Journal of Nutrition, 147(9), 1722–1728. PubMed.
Karlsen, T., Aamot, I. L., Haykowsky, M., & Rognmo, Ø. (2017). High intensity interval training for maximizing health outcomes. Progress in Cardiovascular Diseases, 60(1), 67–77. Crossref. PubMed.
Katzmarzyk, P. T., Church, T. S., Craig, C. L., & Bouchard, C. (2009). Sitting time and mortality from all causes, cardiovascular disease, and cancer. Medicine & Science in Sports & Exercise, 41, 998–1005. Crossref. PubMed.
Kawakami, Y., Akima, H., Kubo, K., Muraoka, Y., Hasegawa, H., Kouzaki, M., … Fukunaga, T. (2001). Changes in muscle size, architecture, and neural activation after 20 days of bed rest with and without resistance exercise. European Journal of Applied Physiology, 84(1–2), 7–12. Crossref. PubMed.
Kilroe, S. P., Fulford, J., Jackman, S. R., Van Loon, L. J. C., & Wall, B. T. (2020). Temporal muscle-specific disuse atrophy during one week of leg immobilization. Medicine & Science in Sports & Exercise, 52(4), 944–954.Crossref. PubMed.
Knudsen, S. H., Hansen, L. S., Pedersen, M., Dejgaard, T., Hansen, J., Hall, G. V., … Krogh-Madsen, R. (2012). Changes in insulin sensitivity precede changes in body composition during 14 days of step reduction combined with overfeeding in healthy young men. Journal of Applied Physiology, 113, 7–15. Crossref. PubMed.
Krebs, J. M., Schneider, V. S., Evans, H., Kuo, M. C., & LeBlanc, A. D. (1990). Energy absorption, lean body mass, and total body fat changes during 5 weeks of continuous bed rest. Aviation, Space and Environmental Medicine, 61, 314–318. PubMed.
Krogh-Madsen, R., Thyfault, J. P., Broholm, C., Mortensen, O. H., Olsen, R. H., Mounier, R., … Pedersen, B. K. (2010). A 2-wk reduction of ambulatory activity attenuates peripheral insulin sensitivity. Journal of Applied Physiology, 108, 1034–1040. Crossref. PubMed.
Kwon, O. S., Tanner, R. E., Barrows, K. M., Runtsch, M., Symons, J. D., Jalili, T., … Drummond, M. J. (2015). Myd88 regulates physical inactivity-induced skeletal muscle inflammation, ceramide biosynthesis signaling, and glucose intolerance. American Journal of Physiology-Endocrinology and Metabolism, 309, E11–E21. Crossref. PubMed.
Kyle, U. G., Morabia, A., Schutz, Y., & Pichard, C. (2004). Sedentarism affects body fat mass index and fat-free mass index in adults aged 18 to 98 years. Nutrition, 20(3), 255–260. Crossref. PubMed.
Larsen, S., Lundby, A.-K. M., Dandanell, S., Oberholzer, L., Keiser, S., Andersen, A. B., … Lundby, C. (2018). Four days of bed rest increases intrinsic mitochondrial respiratory capacity in young healthy males. Physiological Reports, 6(18), e13793. Crossref. PubMed.
Lipman, R. L., Schnure, J. J., Bradley, E. M., & Lecocq, F. R. (1970). Impairment of peripheral glucose utilization in normal subjects by prolonged bed rest. Journal of Laboratory and Clinical Medicine, 76, 221–230. PubMed.
Lovejoy, J. C., Smith, S. R., Zachwieja, J. J., Bray, G. A., Windhauser, M. M., Wickersham, P. J., … de la Bretonne, J. A. (1999). Low-dose T(3) improves the bed rest model of simulated weightlessness in men and women. American Journal of Physiology, 277(2), E370–E379. PubMed.
Lu, S. C. (1999). Regulation of hepatic glutathione synthesis: Current concepts and controversies. The FASEB Journal, 13, 1169–1183. Crossref. PubMed.
Macfarlane, D. J., Taylor, L. H., & Cuddihy, T. F. (2006). Very short intermittent vs continuous bouts of activity in sedentary adults. Preventive Medicine, 43(4), 332–336. Crossref. PubMed.
Matthews, C. E., George, S. M., Moore, S. C., Bowles, H. R., Blair, A., Park, Y., … Schatzkin, A. (2012). Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. The American Journal of Clinical Nutrition, 95(2), 437–445. Crossref. PubMed.
Mazzucco, S., Agostini, F., Mangogna, A., Cattin, L., & Biolo, G. (2010). Prolonged inactivity up-regulates cholesteryl ester transfer protein independently of body fat changes in humans. The Journal of Clinical Endocrinology & Metabolism, 95(5), 2508–2512. Crossref. PubMed.
McGlory, C., von Allmen, M. T., Stokes, T., Morton, R. W., Hector, A. J., Lago, B. A., … Phillips, S. M. (2018). Failed recovery of glycemic control and myofibrillar protein synthesis with 2 wk of physical inactivity in overweight, prediabetic older adults. The Journals of Gerontology: Series A, 73, 1070–1077. Crossref. PubMed.
Mikines, K. J., Richter, E. A., Dela, F., & Galbo, H. (1991). Seven days of bed rest decrease insulin action on glucose uptake in leg and whole body. Journal of Applied Physiology, 70(3), 1245–1254. Crossref. PubMed.
Mikus, C. R., Oberlin, D. J., Libla, J. L., Taylor, A. M., Booth, F. W., & Thyfault, J. P. (2012). Lowering physical activity impairs glycemic control in healthy volunteers. Medicine & Science in Sports & Exercise, 44, 225–231.Crossref. PubMed.
Mindikoglu, A. L., Abdulsada, M. M., Jain, A., Choi, J. M., Jalal, P. K., Devaraj, S., … Jung, S. Y. (2020). Intermittent fasting from dawn to sunset for 30 consecutive days is associated with anticancer proteomic signature and upregulates key regulatory proteins of glucose and lipid metabolism, circadian clock, DNA repair, cytoskeleton remodeling, immune system and cognitive function in healthy subjects. Journal of Proteomics, 217, 103645.Crossref. PubMed.
Miotto, P. M., McGlory, C., Bahniwal, R., Kamal, M., Phillips, S. M., & Holloway, G. P. (2019). Supplementation with dietary omega-3 mitigates immobilization-induced reductions in skeletal muscle mitochondrial respiration in young women. The FASEB Journal, 33, 8232–8240. Crossref. PubMed.
Moro, T., Brightwell, C. R., Deer, R. R., Graber, T. G., Galvan, E., Fry, C. S., … Rasmussen, B. B. (2018). Muscle protein anabolic resistance to essential amino acids does not occur in healthy older adults before or after resistance exercise training. The Journal of Nutrition, 148(6), 900–909. Crossref. PubMed.
Moro, T., Tinsley, G., Bianco, A., Marcolin, G., Pacelli, Q. F., Battaglia, G., … Paoli, A. (2016). Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. Journal of Translational Medicine, 14(1), 290. Crossref. PubMed.
Mortensen, B., Friedrichsen, M., Andersen, N. R., Alibegovic, A. C., Hojbjerre, L., Sonne, M. P., … Vaag, A. (2014). Physical inactivity affects skeletal muscle insulin signaling in a birth weight-dependent manner. Journal of Diabetes and Its Complications, 28, 71–78. Crossref. PubMed.
Morton, R. W., McGlory, C., & Phillips, S. M. (2015). Nutritional interventions to augment resistance training-induced skeletal muscle hypertrophy. Frontiers in Physiology, 6, 245. Crossref. PubMed.
Morton, R. W., Murphy, K. T., McKellar, S. R., Schoenfeld, B. J., Henselmans, M., Helms, E., … Phillips, S. M. (2018). A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults. British Journal of Sports Medicine, 52(6), 376–384. Crossref. PubMed.
Mosole, S., Carraro, U., Kern, H., Loefler, S., Fruhmann, H., Vogelauer, M., … Zampieri, S. (2014). Long-term high-level exercise promotes muscle reinnervation with age. Journal of Neuropathology & Experimental Neurology, 73(4), 284–294. Crossref. PubMed.
Mulder, E., Clément, G., Linnarsson, D., Paloski, W. H., Wuyts, F. P., Zange, J., … Rittweger, J. (2015). Musculoskeletal effects of 5 days of bed rest with and without locomotion replacement training. European Journal of Applied Physiology, 115(4), 727–738. Crossref. PubMed.
Muñoz-Martínez, F. A., Rubio-Arias, JÁ, Ramos-Campo, D. J., & Alcaraz, P. E. (2017). Effectiveness of resistance circuit-based training for maximum oxygen uptake and upper-bodyone-repetition maximum improvements: A Systematic review and meta-analysis. Sports Medicine, 47(12), 2553–2568. Crossref. PubMed.
Myers, J., Prakash, M., Froelicher, V., Do, D., Partington, S., & Atwood, J. E. (2002). Exercise capacity and mortality among men referred for exercise testing. New England Journal of Medicine, 346, 793–801. Crossref. PubMed.
Myllynen, P., Koivisto, V. A., & Nikkila, E. A. (1987). Glucose intolerance and insulin resistance accompany immobilization. Acta Medica Scandinavica, 222, 75–81. Crossref. PubMed.
Nagaya, N., Itoh, T., Murakami, S., Oya, H., Uematsu, M., Miyatake, K., & Kangawa, K. (2005). Treatment of cachexia with ghrelin in patients with COPD. Chest, 128(3), 1187–1193. Crossref. PubMed.
Narici, M., Monti, E., Franchi, M., Sarto, F., Reggiani, C., Toniolo, L., … Pisot, R. (2020). Biomarkers of muscle atrophy and of neuromuscular maladaptation during 10-day bed rest. European Journal of Translational Myology, 30(1), 23–24.
Nishimune, H., Stanford, J. A., & Mori, Y. (2014). Role of exercise in maintaining the integrity of the neuromuscular junction. Muscle & Nerve, 49(3), 315–324. Crossref. PubMed.
O'Keefe, J. H., Vogel, R., Lavie, C. J., & Cordain, L. (2010). Achieving hunter-gatherer fitness in the 21(st) century: Back to the future. The American Journal of Medicine, 123(12), 1082–1086. Crossref. PubMed.
Olsen, R. H., Krogh-Madsen, R., Thomsen, C., Booth, F. W., & Pedersen, B. K. (2008). Metabolic responses to reduced daily steps in healthy nonexercising men. JAMA, 299, 1261–1263. Crossref. PubMed.
Op’t, E. B., Urso, B., Richter, E. A., Greenhaff, P. L., & Hespel, P. (2001). Effect of oral creatine supplementation on human muscle GLUT4 protein content after immobilization. Diabetes, 50, 18–23. Crossref. PubMed.
Paddon-Jones, D., Sheffield-Moore, M., Cree, M. G., Hewlings, S. J., Aarsland, A., Wolfe, R. R., & Ferrando, A. A. (2006). Atrophy and impaired muscle protein synthesis during prolonged inactivity and stress. The Journal of Clinical Endocrinology & Metabolism, 91(12), 4836–4841. Crossref. PubMed.
Panahi, S., & Tremblay, A. (2018). Sedentariness and health: Is sedentary behavior more than just physical inactivity? Frontiers in Public Health, 6, 258. Crossref. PubMed.
Paoli, A., Tinsley, G., Bianco, A., & Moro, T. (2019). The influence of meal frequency and timing on health in humans: The role of fasting. Nutrients, 11(4), 719. Crossref.
Pearson, S. J., Young, A., Macaluso, A., Devito, G., Nimmo, M. A., Cobbold, M., & Harridge, S. D. (2002). Muscle function in elite master weightlifters. Medicine & Science in Sports & Exercise, 34(7), 1199–1206. Crossref. PubMed.
Pedersen, B. K., & Saltin, B. (2015). Exercise as medicine – evidence for prescribing exercise as a therapy in 26 different chronic diseases. Scandinavian Journal of Medicine & Science in Sports, 25(Suppl. 3), 1–72. Crossref. PubMed.
Phillips, R. L., Lemon, F. R., Beeson, W. L., & Kuzma, J. W. (1978). Coronary heart disease mortality among seventh-day adventists with differing dietary habits: A preliminary report. The American Journal of Clinical Nutrition, 31(10 Suppl), S191–S198. Crossref. PubMed.
Pišot, R., Marusic, U., Biolo, G., Mazzucco, S., Lazzer, S., Grassi, B., … Šimunič, B. (2016). Greater loss in muscle mass and function but smaller metabolic alterations in older compared to younger men following two weeks of bed rest and recovery. Journal of Applied Physiology, 120, 922–929. Crossref. PubMed.
Podrez, E. A., Abu-Soud, H. M., & Hazen, S. L. (2000). Myeloperoxidase-generated oxidants and atherosclerosis. Free Radical Biology and Medicine, 28, 1717–1725. Crossref. PubMed.
Porcelli, S., Rasica, L., Zuccarelli, L., Magnesa, B., Degano, C., Comelli, M., … Grassi, B. (2020, May 26–30). Effects of 10-day bed-rest on nitric oxide metabolites and microvascular function assessed by near-infared spectroscopy. 67th annual meeting, American College of Sports Medicine, San Francisco, CA.
Powers, S. K., Kavazis, A. N., & McClung, J. M. (2007). Oxidative stress and disuse muscle atrophy. Journal of Applied Physiology, 102, 2389–2397. Crossref. PubMed.
Pulsford, R. M., Blackwell, J., Hillsdon, M., & Kos, K. (2017). Intermittent walking, but not standing, improves postprandial insulin and glucose relative to sustained sitting: A randomised cross-over study in inactive middle-aged men. Journal of Science and Medicine in Sport, 20, 278–283. Crossref. PubMed.
Pulsford, R. M., Stamatakis, E., Britton, A. R., Brunner, E. J., & Hillsdon, M. (2015). Associations of sitting behaviours with all-cause mortality over a 16-year follow-up: The Whitehall II study. International Journal of Epidemiology, 44(6), 1909–1916. Crossref. PubMed.
Raichlen, D. A., Pontzer, H., Zderic, T. W., Harris, J. A., Mabulla, A. Z. P., Hamilton, M. T., & Wood, B. M. (2020). Sitting, squatting, and the evolutionary biology of human inactivity. Proceedings of the National Academy of Sciences, 117(13), 7115–7121. Crossref. PubMed.
Richards, R. S., Roberts, T. K., Dunstan, R. H., McGregor, N. R., & Butt, H. L. (1998). Erythrocyte antioxidant systems protect cultured endothelial cells against oxidant damage. Biochemistry and Molecular Biology International, 46, 857–865. PubMed.
Richter, E. A., Kiens, B., Mizuno, M., & Strange, S. (1989). Insulin action in human thighs after one-legged immobilization. Journal of Applied Physiology, 67, 19–23. Crossref. PubMed.
Ried-Larsen, M., Aarts, H. M., & Joyner, M. J. (2017). Effects of strict prolonged bed rest on cardiorespiratory fitness: Systematic review and meta-analysis. Journal of Applied Physiology, 123, 790–799. Crossref. PubMed.
Ringholm, S., Bienso, R. S., Kiilerich, K., Guadalupe-Grau, A., Aachmann-Andersen, N. J., Saltin, B., … Pilegaard, H. (2011). Bed rest reduces metabolic protein content and abolishes exercise-induced mRNA responses in human skeletal muscle. American Journal of Physiology-Endocrinology and Metabolism, 301, E649–E658. Crossref. PubMed.
Rittweger, J., & Felsenberg, D. (2009). Recovery of muscle atrophy and bone loss from 90 days bed rest: Results from a one-year follow-up. Bone, 44, 214–224. Crossref. PubMed.
Ritz, P., & Elia, M. (1999). The effect of inactivity on dietary intake and energy homeostasis. Proceedings of the Nutrition Society, 58, 115–122. Crossref. PubMed.
Robertson, M. D., Henderson, R. A., Vist, G. E., & Rumsey, R. D. (2004). Plasma ghrelin response following a period of acute overfeeding in normal weight men. International Journal of Obesity, 28(6), 727–733. Crossref.
Rogers, M. A., King, D. S., Hagberg, J. M., Ehsani, A. A., & Holloszy, J. O. (1990). Effect of 10 days of physical inactivity on glucose tolerance in master athletes. Journal of Applied Physiology, 68(5), 1833–1837. Crossref. PubMed.
Salanova, M., Bortoloso, E., Schiffl, G., Gutsmann, M., Belavy, D. L., Felsenberg, D., … Blottner, D. (2011). Expression and regulation of Homer in human skeletal muscle during neuromuscular junction adaptation to disuse and exercise. The FASEB Journal, 25(12), 4312–4325. Crossref. PubMed.
Salanova, M., Schiffl, G., Püttmann, B., Schoser, B. G., & Blottner, D. (2008). Molecular biomarkers monitoring human skeletal muscle fibres and microvasculature following long-term bed rest with and without countermeasures. Journal of Anatomy, 212, 306–318. Crossref. PubMed.
Saltin, B., Blomqvist, G., Mitchell, J. H., Johnson, R. L., Wildenthal, K., & Chapman, C. B. (1968). Response to exercise after bed rest and after training. Circulation, 38(5 Suppl), 71–78.
Salvadego, D., Keramidas, M. E., Brocca, L., Domenis, R., Mavelli, I., Rittweger, J., … Grassi, B. (2016). Separate and combined effects of a 10-d exposure to hypoxia and inactivity on oxidative function in vivo and mitochondrial respiration ex vivo in humans. Journal of Applied Physiology, 121, 154–163. Crossref. PubMed.
Salvadego, D., Keramidas, M. E., Kölegård, R., Brocca, L., Lazzer, S., Mavelli, I., … Grassi, B. (2018). Planhab*: Hypoxia does not worsen the impairment of skeletal muscle oxidative function induced by bed rest alone. The Journal of Physiology, 596, 3341–3355. Crossref. PubMed.
Schaap, L. A., Pluijm, S. M., Deeg, D. J., & Visser, M. (2006). Inflammatory markers and loss of muscle mass (sarcopenia) and strength. The American Journal of Medicine, 119, 526.e9–526.e17. Crossref. PubMed.
Schaffler, A., Muller-Ladner, U., Scholmerich, J., & Buchler, C. (2006). Role of adipose tissue as an inflammatory organ in human diseases. Endocrine Reviews, 27, 449–467. Crossref. PubMed.
Scheld, K., Zittermann, A., Heer, M., Herzog, B., Mika, C., Drummer, C., & Stehle, P. (2001). Nitrogen metabolism and bone metabolism markers in healthy adults during 16 weeks of bed rest. Clinical Chemistry, 47(9), 1688–1695. Crossref. PubMed.
Shackelford, L. C., LeBlanc, A. D., Driscoll, T. B., Evans, H. J., Rianon, N. J., Smith, S. M., … Lai, D. (2004). Resistance exercise as a countermeasure to disuse-induced bone loss. Journal of Applied Physiology, 97, 119–129. Crossref. PubMed.
Shayt, D. H. (1989). Stairway to redemption: America's encounter with the British prison treadmill. Technology and Culture, 30(4), 908–938. Crossref.
Shook, R. P., Hand, G. A., Drenowatz, C., Hebert, J. R., Paluch, A. E., Blundell, J. E., … Blair, S. N. (2015). Low levels of physical activity are associated with dysregulation of energy intake and fat mass gain over 1 year. The American Journal of Clinical Nutrition, 102(6), 1332–1338. Crossref. PubMed.
Slentz, C. A., Houmard, J. A., & Kraus, W. E. (2007). Modest exercise prevents the progressive disease associated with physical inactivity. Exercise and Sport Sciences Reviews, 35, 18–23. Crossref. PubMed.
Sonne, M. P., Alibegovic, A. C., Hojbjerre, L., Vaag, A., Stallknecht, B., & Dela, F. (2010). Effect of 10 days of bedrest on metabolic and vascular insulin action: A study in individuals at risk for type 2 diabetes. Journal of Applied Physiology, 108, 830–837. Crossref. PubMed.
Sonne, M. P., Hojbjerre, L., Alibegovic, A. C., Nielsen, L. B., Stallknecht, B., Vaag, A. A., & Dela, F. (2011). Endothelial function after 10 days of bed rest in individuals at risk for type 2 diabetes and cardiovascular disease. Experimental Physiology, 96, 1000–1009. Crossref. PubMed.
Srikanthan, P., & Karlamangla, A. S. (2014). Muscle mass index as a predictor of longevity in older adults. The American Journal of Medicine, 127(6), 547–553. Crossref. PubMed.
Stamatakis, E., Hamer, M., & Dunstan, D. W. (2011). Screen-based entertainment time, all-cause mortality, and cardiovascular events: Population-based study with ongoing mortality and hospital events follow-up. Journal of the American College of Cardiology, 57(3), 292–299. Crossref. PubMed.
Stein, T. P., Leskiw, M. J., Schluter, M. D., Donaldson, M. R., & Larina, I. (1999). Protein kinetics during and after long-duration spaceflight on MIR. American Journal of Physiology-Cell Physiology, 276, E1014–E1021.PubMed.
Stevenson, E. J., Giresi, P. G., Koncarevic, A., & Kandarian, S. C. (2003). Global analysis of gene expression patterns during disuse atrophy in rat skeletal muscle. The Journal of Physiology, 551, 33–48. Crossref. PubMed.
Stuart, C. A., Shangraw, R. E., Prince, M. J., Peters, E. J., & Wolfe, R. R. (1988). Bed-rest-induced insulin resistance occurs primarily in muscle. Metabolism, 37, 802–806. Crossref. PubMed.
Stubbs, R. J., Hughes, D. A., Johnstone, A. M., Horgan, G. W., King, N., & Blundell, J. E. (2004). A decrease in physical activity affects appetite, energy, and nutrient balance in lean men feeding ad libitum. The American Journal of Clinical Nutrition, 79(1), 62–69. Crossref. PubMed.
Suchomel, T. J., Nimphius, S., Bellon, C. R., & Stone, M. H. (2018). The importance of muscular strength: Training considerations. Sports Medicine, 48(4), 765–785. Crossref. PubMed.
Suetta, C., Hvid, L. G., Justesen, L., Christensen, U., Neergaard, K., Simonsen, L., … Aagaard, P. (2009). Effects of aging on human skeletal muscle after immobilization and retraining. Journal of Applied Physiology, 107(4), 1172–1180. Crossref. PubMed.
Tabata, I., Suzuki, Y., Fukunaga, T., Yokozeki, T., Akima, H., & Funato, K. (1999). Resistance training affects GLUT-4 content in skeletal muscle of humans after 19 days of head-down bed rest. Journal of Applied Physiology, 86, 909–914. Crossref. PubMed.
Tanimoto, M., & Ishii, N. (2006). Effects of low-intensity resistance exercise with slow movement and tonic force generation on muscular function in young men. Journal of Applied Physiology, 100(4), 1150–1157. Crossref. PubMed.
Tesch, P. A., von Walden, F., Gustafsson, T., Linnehan, R. M., & Trappe, T. A. (2008). Skeletal muscle proteolysis in response to short-term unloading in humans. Journal of Applied Physiology, 105(3), 902–906. Crossref. PubMed.
Thyfault, J. P., & Krogh-Madsen, R. (2011). Metabolic disruptions induced by reduced ambulatory activity in free-living humans. Journal of Applied Physiology, 111(4), 1218–1224. Crossref. PubMed.
Trappe, S., Creer, A., Slivka, D., Minchev, K., & Trappe, T. (2007). Single muscle fiber function with concurrent exercise or nutrition countermeasures during 60 days of bed rest in women. Journal of Applied Physiology, 103(4), 1242–1250. Crossref. PubMed.
Tremblay, M. S., Aubert, S., Barnes, J. D., Saunders, T. J., Carson, V., Latimer-Cheung, A. E., … Altenburg, T. M. (2017). Sedentary behavior research network (SBRN) – terminology consensus project process and outcome. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 75. Crossref. PubMed.
Tudor-Locke, C., Craig, C. L., Thyfault, J. P., & Spence, J. C. (2013). A step-defined sedentary lifestyle index: <5000 steps/day. Applied Physiology, Nutrition, and Metabolism, 38, 100–114. Crossref. PubMed.
Van der Ploeg, H. P., Chey, T., Korda, R. J., Banks, E., & Bauman, A. (2012). Sitting time and all-cause mortality risk in 222 497 Australian adults. Archives of Internal Medicine, 172, 494–500. Crossref. PubMed.
Van Guilder, G. P., Hoetzer, G. L., Greiner, J. J., Stauffer, B. L., & Desouza, C. A. (2006). Influence of metabolic syndrome on biomarkers of oxidative stress and inflammation in obese adults. Obesity, 14, 2127–2131. Crossref. PubMed.
Vasconcelos, A. R., Yshii, L. M., Viel, T. A., Buck, H. S., Mattson, M. P., Scavone, C., & Kawamoto, E. M. (2014). Intermittent fasting attenuates lipopolysaccharide-induced neuroinflammation and memory impairment. Journal of Neuroinflammation, 11, 85. Crossref. PubMed.
Volpi, E., Campbell, W. W., Dwyer, J. T., Johnson, M. A., Jensen, G. L., Morley, J. E., & Wolfe, R. R. (2013). Is the optimal level of protein intake for older adults greater than the recommended dietary allowance? The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 68(6), 677–681. Crossref. PubMed.
Vukovich, M. D., Arciero, P. J., Kohrt, W. M., Racette, S. B., Hansen, P. A., & Holloszy, J. O. (1996). Changes in insulin action and GLUT-4 with 6 days of inactivity in endurance runners. Journal of Applied Physiology, 80, 240–244. Crossref. PubMed.
Wade, C. E., Miller, M. M., Baer, L. A., Moran, M. M., Steele, M. K., & Stein, T. P. (2002). Body mass, energy intake, and water consumption of rats and humans during space flight. Nutrition, 18, 829–836. Crossref. PubMed.
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729.Crossref.
Westerterp, K. R. (2003). Impacts of vigorous and non-vigorous activity on daily energy expenditure. Proceedings of the Nutrition Society, 62(3), 645–650. Crossref. PubMed.
Wilmot, E. G., Edwardson, C. L., Achana, F. A., Davies, M. J., Gorely, T., Gray, L. J., … Biddle, S. J. (2012). Sedentary time in adults and the association with diabetes, cardiovascular disease and death: Systematic review and meta-analysis. Diabetologia, 55(11), 2895–2905. Crossref. PubMed.
Wilson, M. M., & Morley, J. E. (2003). Aging and energy balance. Journal of Applied Physiology, 95, 1728–1736.Crossref. PubMed.
Zuccarelli, L., Magnesa, B., Degano, C., Comelli, M., Gasparini, M., Manferdelli, G., … Grassi, B. (2020, May 26–30). The impairment of oxidative metabolism during exercise after 10 days of bed rest is upstream of skeletal muscle mitochondria. 67th annual meeting, American College of Sports Medicine, San Francisco, CA.